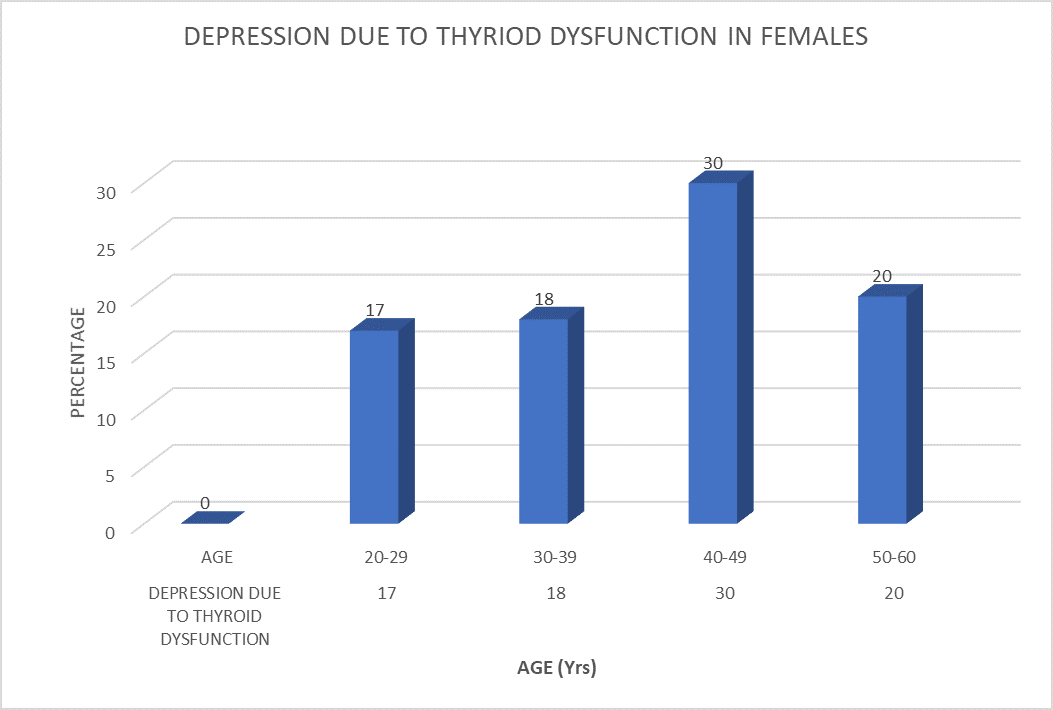
Introduction:Psychiatry:Psychiatry is the branch of medicine focused on the diagnosis, treatment and prevention of mental, emotional and behavioural disorders.Depression is a prevalent mental illness. An estimated 5% of adults worldwide are depressed. Depression affects more women than males. Suicide can result from depression. Depression, whether mild, moderate, or severe, can be effectively treated. The thyroid is a little gland at the front of your neck that resembles a butterfly. It produces hormones that regulate the body's energy consumption. These hormones regulate almost all of your body's vital processes and have an impact on almost every organ. Thyroid hormone imbalances, whether from excess or insufficiency, can lead to mood disorders, such as depression, which can be effectively treated with thyroid medication. A prospective cohort study is a kind of observational research that tracks a cohort of individuals throughout time to gather information on their exposure to a factor of interest.Materials And Methods:Place of study:The study “a prospective study on depression due to thyroid dysfunction’’ which was carried out in the Department of Psychiatry at Narayana Hospital, Nellore, in collaboration with a 1200 bedded multidisciplinary teaching hospital, under the guidance of dr .sasi kala mam. pharm d asistant professor of Narayana pharmacy college, Department of Pharmacy Practise, Narayana Medical college, Nellore.Study design:The study was a prospective observational clinical study in the Department of Psychiatry of tertiary care teaching hospitals.Study population:This study was conducted in 200 patients who came to the department of Psychiatry and General Medicine with the complications of depression due to Thyroid DysfunctionStudy durations:This study was conducted for a period of 6 months (September 2023-Feburary 2024)Results:Here in this study, we have collected the data from Psychiatry department. In this study maximum number patients reported in the Psychiatry department. Most of the people is suffering from the depression due Thyroid dysfunction. Females are more affected than males Discussion:The patients are mostly covered from the Psychiatry department most of the people are suffering from the depression due to the thyroid dysfunction in adults.They were treated anti thyroid medication and antidepression medication. Our study is about Depression due to Thyroid dysfunction with its clinical approach in which the data was collected from the patients by using HMD scale of Depression.Out of 200 patients, 130 patients were suitable for study based on inclusion and exclusion criteria.In our study we have categorized the patients using Depression due Thyroid dysfunction.Out of 200 patients 130 patients considered for the study, mostly were females i.e .85(65%) and males are fewer i.e.45(35%)among the age groups of 20-60 .Patients were categorized based on their age groups and gender in which majority of them 30(36%) females were found in the between 40-50 years ,17(20%) in between 20-29years ,18 (21%) in between 30-39years ,24(20%)in between 50-60 years.In males majority were found in 15(33%) in between the age groups 40-49. 12 (27%) in between in age groups of 20-29.14(31%) in between in age groups of 30-39 .15(33%) in between in the age groups of 40-49. 4(9%) in the between age groups 50-60.conclusion:Our study concluded that most of the patients admitted in the Psychiatry department. Depression due to Thyroid dysfunction the production of neurotransmitters is slow so it leads Depression in Thyroid Dysfunction The synthesis and operation of neurotransmitters in the brain, such as serotonin, which is connected to mood regulation, may be impacted by low thyroid hormone levels.
Depression, Thyroid dysfunction, Hypothyroidism, Hyperthyroidism, Mood disorders, Hamilton Depression Rating Scale (HDRS), Neurotransmitters, Psychiatry, Prospective study, Mental health, Endocrinology, Gender disparity, Combined therapy, Hormonal imbalance, Clinical outcomes
1.1.DEPRESSION:
Depression is a common mental disorder. Globally, an estimated 5% of adults suffer from depression. More women are affected by depression than men. Depression can lead to suicide. There is effective treatment for mild, moderate and severe depression.
1.1.2Key features depression may include:
1.Persistant feeling of sadness: People who are depressed frequently feel a constant sense of melancholy or emptiness that lasts for a long time—two weeks or longer.
2. Loss of interest: One common symptom is a marked decline in interest or enjoyment in once-enjoyable activities. Isolation and social disengagement may result from this.
3.Changes in sleep pattern: Sleep patterns can be disturbed by depression, which can result in excessive or insomniac sleeping.
4.Fatigue and lack of energy: Depression can cause a person to feel exhausted all the time and lacking in energy to do daily tasks.
5.Difficulty concentrating: Concentration, decision-making, and memory are problems that many depressed people face.
6.Change in appetite or weight: Changes in eating patterns brought on by depression may cause substantial weight gain or loss.
7.Feeling worthlessness and Guilt: Even in the absence of a logical explanation, depressed people may harbour enduring feelings of guilt or worthlessness.
8.Physical symptoms: A headache, stomach problems, or unexplained aches and pains are examples of physical symptoms that some people with depression may also experience.
9.Sucidial symptoms: Severe depression can result in suicidal or fatal thoughts. It's critical to get help right away if you or someone you know is having suicidal thoughts.
1.1.3What are the types of depression? Depressive disorders are categorised as follows in the Diagnostic and Statistical Manual of Mental Disorders; Fifth Edition (DSM-5) published by the American Psychiatric Association
1.Clinical depression (major depressive
disorders):A severe depressive disorder diagnosis indicates that you have had symptoms such as changes in appetite, difficulty sleeping, and loss of interest in activities on most days for at least two weeks, along with feelings of sadness, worthlessness, or melancholy. This is one of the most prevalent and severe types of depression.
2.Persistant Depressive disorder:
Mild to severe depression that persists for two years or longer is known as persistent depressive disorder. Compared to major depressive illness, the symptoms are not as severe. PDD dysthymia was the term used by medical professionals.
3.Desruptive mood dysregulation disorders:
Children with severe, persistent irritability and frequent episodes of anger are diagnosed with DMDD. By age 10, symptoms typically start to appear.
4.Premenstural dysphoric disorder (PMDD):
Premenstrual syndrome (PMS) symptoms, such as severe irritability, anxiety, or depression, coexist with mood problems when you have PMDD. After your period begins, these symptoms usually go away in a few days, but sometimes they might be so bad that they interfere with your daily activities.
5.Depressive disorders due to another medical condition: Depression can be brought on by a variety of medical problems that alter your body. Cancer, heart disease, Parkinson's disease, and hypothyroidism are a few examples. When the underlying illness is successfully treated, depression typically gets better as well. They are also some specific forms of major depressive disorders, including: Seasonal affective disorders (seasonal depression):This type of significant depression usually appears in the fall and winter and disappears in the spring and summer. Prenatal depression and postpartum disorders: Depression that develops during pregnancy is known as prenatal depression. Depression known as postpartum depression appears four weeks after giving birth. "Major depressive disorder (MDD) with peripartum onset" is how the DSM describes these conditions.
Psychotic depression:
In addition to the "psychotic" symptoms of major depression, people with psychotic depression also experience the following symptoms:
Hallucinations: the perception of unreal sounds or sights.Delusions, or mistaken beliefs.The false belief that someone is attempting to harm you is known as paranoia. Psychotic depression can be treated with antipsychotic and antidepressant medications together. ECT is another possible option.
Situational depression:
In psychiatry, this is not a technical term. However, you may experience depression if you're finding it difficult to cope with a life-threatening incident, such a divorce, a death in the family, or losing your work. Your physician might refer to this as "stress response syndrome
Atypical depression: This kind differs from the chronic melancholy of a regular depression. It's regarded as a "specifier" that characterizes a subset of depression symptoms. In cases of atypical depression, a happy occasion may momentarily lift your spirits.
Other symptoms of atypical include:
- Increased appetite
- Feeling of heaviness
- Oversensitive to criticism
- Sleeping more than usual
Treatment resistance depression:
One-third of patients receiving treatment for depression attempt many approaches without finding improvement. If so, you may have depression that is resistant to treatment. Your depression may not respond to treatment for a variety of reasons. For instance, treating your depression may be challenging due to other medical issues you may have.In the event that your doctor diagnoses you with treatment-resistant depression, they may suggest some unconventional therapy approaches. In certain cases, electroconvulsive treatment (ECT) is beneficial.
1.1.4etiolgy:Major depressive illness is thought to have a complex etiology involving biological, genetic, environmental, and psychological components. Serotonin, norepinephrine, and dopamine problems in particular were thought to be the primary causes of MDD in the past. The use of many antidepressants, including dopamine-norepinephrine receptor inhibitors, selective serotonin receptor inhibitors, and serotonin-norepinephrine receptor inhibitors, in the treatment of depression, has demonstrated this. Serotonin metabolites have been discovered to be reduced in people who experience suicidal thoughts. Nevertheless, current hypotheses suggest that it is mostly linked to intricate brain circuits and neuroregulatory systems, which in turn lead to secondary disruptions of neurotransmitter systems.Depression's genesis has been linked to glutamate and glycine, two important excitatory neurotransmitters, as well as the inhibitory neurotransmitter GABA. Lower levels of brain GABA, CSF, and plasma have been observed in depressed people. GABA is thought to work as an antidepressant by blocking the mesolimbic and mesocortical systems, two ascending monoamine routes. Antidepressant effects have been studied for medications that bind to NMDA receptors. The etiology of mood disorders has also been linked to changes in growth hormone and thyroid function. Depression in adult life is linked to a history of traumatic experiences and unfavourable childhood circumstances. A lifetime of severe depression can be caused by profound changes in neuroendocrine and behavioural responses brought on by extreme early stress. These changes can also result in anatomical modifications in the cerebral cortex. Increased hyperintensities in the subcortical areas and decreased anterior brain metabolism on the left side have been observed in structural and functional brain imaging of sad patients. Studies on families, adoption, and twins have shown that genes have a part in a person's propensity for depression. The concordance rate of MDD in twins, especially monozygotic twins, is exceptionally high, according to genetic studies. Psychological characteristics and life experiences have also been demonstrated to be significant. Depression has been linked to experiencing uncontrollable situations, according to the learned helplessness idea. According to cognitive theory, for those who are predisposed to depression, depression results from cognitive distortions.
1.1.5epidemilogy:One very common mental illness is major depressive disorder. The average lifetime prevalence is 12 percent, and it ranges from 5 to 17 percent. In women compared to men, the prevalence rate is nearly twice as high. It has been suggested that this discrepancy results from hormonal variations, the consequences of childbirth, the fact that men and women experience distinct psychosocial pressures, and the behavioural concept of learned helplessness. Despite the average age of beginning being approximately 40 years old, current surveys indicate a growing incidence in younger populations as a result of alcohol and other substance addiction.
People lacking deep interpersonal interactions, as well as those who are bereaved, divorced, or separated, are more likely to suffer from MDD. There is no discernible variation in the prevalence of MDD based on socioeconomic class or race. Comorbid conditions include drug use disorders, panic attacks, social anxiety, and obsessive-compulsive disorder are frequently present in people with major depressive disorder (MDD). Those with MDD who also suffer from these comorbid conditions have a higher risk of suicide. Depression is common in older persons who also have co-occurring medical conditions. Research indicates that depression is more common in rural than in urban regions.
1.1.6symptomS:
Individuals may experience:
Mood: apathy, general discontent, guilt, anxiety, hopelessness, loss of interest or pleasure in activities, mood swings, or sadness
Sleep: early awaking, excess sleepiness, insomnia, or restless sleep,
Whole body: excessive hunger, fatigue, loss of appetite, or social isolation
Cognitive: lack of concentration, slowness in activity, or thoughts of suicide
Weight: weight gain, weight loss
Also common: poor appetite or repeatedly going over thoughts (9)
1.1.7Differential diagnosis:Hamilton depression rating scale:The most popular interview tool is the Hamilton Depression Rating Scale, which was created in 1960 to gauge the severity of depression in a patient population confined to an inpatient facility. Numerous iterations have been developed since then, such as computerized versions, self-report forms, and structured interview guides. Items 18–21 are used to further qualify the depression in the original clinician-administered scale, while the first 17 items are tallied for the overall score. It takes 20 to 30 minutes to administer the scale. A score between 0 and 7 is regarded as normal, while a score of 20 or above denotes moderately severe depression. Each item is rated on a 3-point scale, which denotes absent, slight or questionable, and clearly present symptoms, or on a 5-point scale, which represents non existent, mild, moderate, or severe symptoms. There are comparatively few cognitive or affective symptoms in the HDRS compared to a high number of physical symptoms.The scale is based on a structured interview:
1 Depressed Mood (sadness, hopeless, helpless, worthless)
0 |__| Absent.
1 |__| These feeling states indicated only on questioning.
2 |__| These feeling states spontaneously reported verbally.
3 |__| Communicates feeling states non-verbally, i.e. through facial expression, posture, voice and tendency to weep.
4 |__| Patient reports virtually only these feeling states in his/her spontaneous verbal and non-verbal communication.
2 Feelings Of Guilt
0 |__| Absent.
1 |__|Self reproach, feels he/she has let people down.
2 |__| Ideas of guilt or rumination over past errors or sinful deeds.
3 |__| Present illness is a punishment. Delusions of guilt.
4 |__| Hears accusatory or denunciatory voices and/or experiences threatening visual hallucinations.
3 Suicide
0 |__| Absent.
1 |__| Feels life is not worth living.
2 |__| Wishes he/she were dead or any thoughts of possible death to self.
3 |__| Ideas or gestures of suicide.
4 |__| Attempts at suicide (any serious attempt rate 4).
4 Insomnia: Early In The Night
0 |__| No difficulty falling asleep.
1 |__| Complains of occasional difficulty falling asleep, i.e. more than 1 ?2 hour.
2 |__| Complains of nightly difficulty falling asleep.
5 Insomnia: Middle Of The Night
0 |__| No difficulty.
1|__| Patient complains of being restless and disturbed during the night.
2 |__| Waking during the night – any getting out of bed rates 2 (except for purposes of voiding).
6 Insomnia: Early Hours Of The Morning
0 |__| No difficulty.
1 |__| Waking in early hours of the morning but goes back to sleep.
2 |__| Unable to fall asleep again if he/she gets out of bed.
7 Work And Activities
0 |__| No difficulty.
1 |__| Thoughts and feelings of incapacity, fatigue or weakness related to activities, work or hobbies.
2 |__| Loss of interest in activity, hobbies or work – either directly reported by the patient or indirect in listlessness, indecision and vacillation (feels he/she has to push self to work or activities).
3 |__| Decrease in actual time spent in activities or decrease in productivity.
Rate 3 if the patient does not spend at least three hours a day in activities (job or hobbies) excluding routine chores.
4 |__| Stopped working because of present illness. Rate 4 if patient engages in no activities except routine chores, or if patient fails to perform routine chores unassisted.
8 Retardation (slowness of thought and speech, impaired ability to concentrate, decreased motor activity)
0 |__| Normal speech and thought.
1 |__| Slight retardation during the interview.
2 |__| Obvious retardation during the interview.
3 |__| Interview difficult.
4 |__| Complete stupor.
9 Agitation
0 |__| None.
1 |__| Fidgetiness.
2 |__| Playing with hands, hair, etc.
3 |__| Moving about, can’t sit still.
4 |__| Hand wringing, nail biting, hair-pulling, biting of lips.
10 Anxiety Psychic
0 |__| No difficulty.
1 |__| Subjective tension and irritability.
2 |__| Worrying about minor matters.
3 |__| Apprehensive attitude apparent in face or speech.
4 |__| Fears expressed without questioning.
11 Anxiety Somatic (physiological concomitants of anxiety)such as: gastro-intestinal – dry mouth, wind, indigestion, diarrhea, cramps, belching cardio-vascular – palpitations, headaches respiratory – hyperventilation, sighing urinary frequency sweating
0 |__| Absent.
1 |__| Mild.
2 |__| Moderate.
3 |__| Severe.
4 |__| Incapacitating.
12 Somatic Symptoms Gastro-Intestinal
0 |__| None.
1 |__| Loss of appetite but eating without staff encouragement. Heavy feelings in abdomen.
2 |__| Difficulty eating without staff urging. Requests or requires laxatives or medication for bowels or medication for gastro-intestinal symptoms.
13 General Somatic Symptoms
0 |__| None.
1 |__| Heaviness in limbs, back or head. Backaches, headaches, muscle aches. Loss of energy and fatigability.
2 |__| Any clear-cut symptom rates 2.
14 Genital Symptoms (symptoms such as loss of libido, menstrual disturbances)
0 |__| Absent.
1 |__| Mild.
2 |__| Severe.
15 Hypochondriasis
0 |__| Not present.
1 |__| Self-absorption (bodily).
2 |__| Preoccupation with health.
3 |__| Frequent complaints, requests for help, etc.
4 |__| Hypochondriacal delusions.
16 Loss Of Weight (Rate Either A Or B)
According to the measurements:
0 |__| No weight loss.
1 |__| Probable weight
2 |__| Definite (according to patient weight loss weight in week. loss.
3 |__| Not assessed.
According to weekly patient: measurements:
0 |__| Less than 1 lb weight loss in week.
1 |__| Greater than 1 lb weight loss loss in week
2 |__| Greater than 2 lb weight loss in week. loss.
3 |__| Not assessed.
17 Insight
0 |__| Acknowledges being depressed and ill.
1 |__| Acknowledges illness but attributes cause to bad food, climate, overwork, virus, need for rest, etc.
2 |__| Denies being ill at all.
Total score: |__|__| 8
1.1.8 Treatment:
Depression is one of the most treatable mental health conditions. Approximately 80% to 90% of people with depression who seek treatment eventually respond well to treatment.
Psychotherapy: Speaking with a mental health professional is the goal of psychotherapy, sometimes known as talk therapy. Your therapist assists you in recognizing and altering negative feelings, ideas, and actions. Psychotherapy comes in numerous forms, the most popular of which is cognitive behavioural treatment, or CBT. Sometimes you just need short-term counselling. Some people stay in therapy for a few months or even years.
Medication: Antidepressants, a class of prescription drugs, can help alter the brain chemistry that underlies depression. Finding the antidepressant that works best for you may take some time because there are various varieties. The side effects of several antidepressants frequently go better over time. Speak with your healthcare provider if they don't. A different prescription could be more effective for patient.
Treatments that you might receive in addition to conventional Western medicine are referred to as complementary medicine. Biofeedback, acupuncture, massage, hypnosis, and other therapies can help people who are suffering from persistent symptoms of mild depression or enhance their overall well-being.
Brain Stimulation Therapy: Individuals with severe depression or psychotic depression may benefit from brain stimulation therapy. Vagus nerve stimulation (VNS), transcranial magnetic stimulation (TMS), and electroconvulsive treatment (ECT) are a few forms of brain stimulation therapy. Additionally, there are activities you may do at home to lessen the symptoms of depression, such as: exercising on a regular basis.
Sleeping well—not too little, not too much. consuming a balanced diet.
staying away from alcohol, which depresses.
interacting with those that are important to you.
1.2thyroid:
Being an endocrine gland, the thyroid. It is located in the inferior, anterior neck and is in charge of maintaining iodine homeostasis in the human body in addition to forming and secreting thyroid hormones. About 90% of the inactive thyroid hormone, or thyroxine (T4), and 10% of the active thyroid hormone, or triiodothyronine (T3), are produced by the thyroid. Peripherally, inactive thyroid hormone is transformed into one of two forms: alternative inactive thyroid hormone or activated thyroid hormone.
1.2.1development:
At the conclusion of the fourth week of development, the thyroid diverticulum initially appears as a solid, growing mass of endoderm at the foramen cecum on the tongue-destined tissue. Through the thyroglossal duct, this mass of endoderm migrates down through the growing neck toward its final location, which is directly inferior to the cricoid cartilage. By the conclusion of the fifth week, the thyroglossal duct deteriorates in a normal development. The foramen cecum, located at the base of the matured tongue, is the lone remnant of the thyroid's embryonic growth. By the conclusion of the seventh week of development, the isolated thyroid gland has developed two distinct lobes joined by a tissue isthmus, is still descending, and has arrived at its goal. The parafollicular cells, or C cells, that will create calcitonin are formed when cells from the ultimobranchial bodies infiltrate the developing thyroid. Neural crest cells invade and produce the thyroid gland s connective tissue.
1.2.2function:
The thyroid gland plays a vital role in maintain the body’s overall metabolic function
Hormone Production : Thyroxine (T4) and triiodothyronine (T3) are the two main hormones produced by the thyroid gland. These hormones are necessary for the body's cells to function properly and contain iodine.
Metabolic regulation:The body's metabolism is regulated by the T3 and T4 hormones, which impact how quickly cells convert food into energy. They regulate the rate at which the body consumes energy, impacting functions including heart rate, temperature control, and burning of calories.
Growth And Development:For healthy growth and development, thyroid hormones are essential, particularly throughout fetal development and childhood. They have an impact on how the skeletal and brain systems grow.
Temperature Regulation:Thyroid hormones affect heat generation and dissipation, which aids in controlling body temperature. They contribute to the preservation of a constant body temperature.
Digestive Function:The speed at which food passes through the digestive tract is one aspect of the digestive system that is influenced by thyroid hormones. They may have an impact on nutrient absorption and appetite.
Heart Rate And Blood Flow:Heart rate and heartbeat intensity are influenced by thyroid hormones. They also have an impact on blood vessel function, which aids in blood pressure regulation.
Muscle control:Thyroid hormones are involved in preserving muscular tone and regulating muscle contraction and relaxation.
Brain Function:These hormones, which have an impact on mood, cognitive performance, and general mental health, are essential for healthy brain function.
Bone health:
Bone formation and maintenance are influenced by thyroid hormones. They are crucial for preserving strong bones and averting ailments like osteoporosis.
Reproductive health: The menstrual cycle and fertility are both regulated by thyroid hormones. They support the reproductive system's regular operation. One can develop hyperthyroidism (an overactive thyroid) or hypothyroidism (an underactive thyroid) as a result of the thyroid gland producing too many or too few hormones. For general health and wellbeing, thyroid hormone equilibrium must be maintained.
1.2.3Mechanism:There are three types of iodothyronines that are produced by the thyroid gland. Triiodothyronine (T3) prohormone inactive thyroxine (T4) is the main secretory product. In tissues like the liver and kidneys with strong blood flow, type 1 deiodinase converts T4 to T3 peripherally. In the brain, glial cells generate type 2 deiodinase, which converts T4 to active T3. Reverse T3, or rT3, is the name given to the third iodothyronine. Type 3 deiodinase activity on T4 generates the inactive rT3. Thyroglobulin and iodine make up these iodothyronines. Inside the thyroid cells, amino acids are arranged from basal to apical to make thyroglobulin. After being secreted into the follicular lumen, thyroglobulin combines with iodine through an enzyme reaction to generate iodinated thyroglobulin. After endosomes carrying this iodinated thyroglobulin fuse with lysosomes, the resulting thyroid hormone's thyroglobulin is released enzymatically. After that, the cell releases the thyroid hormones, and the leftover thyroglobulin is deiodinated and recycled for later use. 1.2.4Diagnostic tools: Thyroid diseases are usually diagnosed by a multidisciplinary team using laboratory testing, medical history, and clinical evaluation. The following essential diagnostic instruments are frequently used to evaluate thyroid function: Thyroid function tests (TFTs)
Thyroid stimulating hormone (TSH):
The pituitary gland secretes TSH, which causes the thyroid to generate T3 and T4. TSH values that are high or low can signify hyperthyroidism or hypothyroidism, respectively.
Free thyroxine (free T4) and Triiodothyronine (free T3):
These assays quantify blood levels of thyroid hormones that are active. Unusual values could point to thyroid issues.
Thyroid imaging:
Ultrasound: The thyroid gland's size, shape, and existence of cysts or nodules can all be seen using an ultrasound.
Radioactive iodine uptake (RAIUs) scan: This test assesses the thyroid's iodine uptake capacity. Diagnoses for thyroid nodules and hyperthyroidism can be made with its assistance.
Antibody tests: Thyroid antibody tests (TPO ANTIBODIES, TGS antibodies)
Thyroid peroxidase (TPO) or thyroglobulin (TG) antibody levels may be elevated in patients with autoimmune thyroid diseases, including Graves' disease and Hashimoto's thyroiditis.
Fine needle aspiration needle (FNA) biopsy: If thyroid nodules are found, a biopsy may be carried out to determine the nodule's benign or malignant nature. In order to examine this, a tiny tissue sample must be removed.
Physical examination: A medical professional may do a physical examination of the thyroid gland to look for nodules, enlargement, or discomfort.
Symptoms assessment: Specific symptoms, such as changes in weight, exhaustion, sensitivity to cold, and alterations in the skin, hair, or nails, can offer more diagnostic hints.
Medical history: Understanding risk factors, family history, and potential triggers for thyroid dysfunction is aided by a comprehensive medical history.It's crucial to remember that thyroid test interpretation frequently calls for knowledge, and medical professionals take into account a number of variables in order to deliver a precise diagnosis. Furthermore, different laboratories may have different normal reference ranges for thyroid function tests, and the results should be interpreted taking into account the patient's overall health and clinical presentation. It's critical to speak with a healthcare provider if you think you may have a thyroid condition or if you are exhibiting symptoms in order to receive an accurate diagnosis and suitable treatment.
1.2.5Pathophysiology:Underproduction of thyroid hormone is the result of an endocrine disease called hypothyroidism. Cold intolerance, weight gain from decreased basal metabolic rate and thermogenesis, depression, exhaustion, diminished peripheral reflexes, and constipation from decreased central and peripheral nervous system stimulation are common symptoms of hypothyroidism. Due to the absence of active thyroid hormone in different human tissues and organs, hypothyroidism can have numerous additional side effects. Excess thyroid hormone production is the hallmark of the endocrine disease hyperthyroidism. Unlike hypothyroidism, hyperthyroidism frequently results in palpitations, heat sensitivity, weight loss, anxiety, hyperreflexia, and diarrhea. The most prevalent symptoms are caused by increased stimulation of the central and peripheral nerve systems, basal metabolic rate, thermogenesis, resting heart rate, and cardiac output. Nonetheless, a wide range of symptoms, such as dry skin, brittle hair, and pretibial myxedema, may appear. There may be extra orbitopathy pathophysiology in Graves disease, an autoimmune disorder in which an auto-antibody activates the TSH-receptor. Additionally, the TSH-receptor antibody stimulates T cells, promotes fibroblast growth, and accumulates glycosaminoglycans in the connective tissue of the retroocular muscles and extraocular muscles, which results in proptosis. The main cause of hypothyroidism, which is connected to HLA-DR5, is Hashimoto thyroiditis. Anti-thyroid peroxidase and anti-thyroglobulin antibodies point to Hashimoto thyroiditis. (14)
1.2.6Symptoms:
Hypothyroidism symptoms:
- Tiredness.
- More sensitivity to cold.
- Constipation.
- Dry skin.
- Weight gain.
- Puffy face.
- Hoarse voice.
- Coarse hair and skin.
- Muscle weakness.
- Muscle aches, tenderness and stiffness.
- Menstrual cycles that are heavier than usual or irregular.
- Thinning hair.
- Slowed heart rate, also called bradycardia.
- Depression.
- Memory problems.
Hyperthyroidism symptoms:
Hyperthyroidism has a wide range of symptoms that can affect every part of your body. Some of these symptoms may affect you more than others, or you may have several of them at once. Hyperthyroidism symptoms can include:
- Losing weight without trying.
- Fast heartbeat, a condition called tachycardia.
- Irregular heartbeat, also called arrhythmia.
- Pounding of the heart, sometimes called heart palpitations.
- Increased hunger.
- Nervousness, anxiety and irritability.
- Tremor, usually a small trembling in the hands and fingers.
- Sweating.
- Changes in menstrual cycles.
- Increased sensitivity to heat.
- Changes in bowel patterns, especially more-frequent bowel movements.
- Enlarged thyroid gland, sometimes called a goiter, which may appear as a swelling at the base of the neck.
- Tiredness.
- Muscle weakness.
- Sleep problems.
- Warm, moist skin.
- Thinning skin.
- Fine, brittle hair.
In older folks, difficult-to-notice symptoms are more common. An irregular heartbeat, weight loss, depression, and fatigue or weakness throughout daily tasks are some of these symptoma
1.2.8 Relation between thyroid anddepression:Thyroid malfunction can, in fact, cause or worsen depressive symptoms. The link between the thyroid and depression is complicated. Thyroxine, or T4, and triiodothyronine, or T3, are the main hormones produced by the thyroid, a butterfly-shaped gland in the neck that are essential for controlling mood and metabolism, among other body processes.
Hypothyroidism and depression:The insufficient production of thyroid hormones by the thyroid gland results in hypothyroidism.Hypothyroidism can cause mood swings, weight gain, exhaustion, and trouble concentrating. In more extreme circumstances, it may exacerbate clinical depression.The synthesis and operation of neurotransmitters in the brain, such as serotonin, which is connected to mood regulation, may be impacted by low thyroid hormone levels.
Hyperthyroidism and depression: The converse condition is called hyperthyroidism, in which the thyroid overproduces hormones. Although anxiety and irritability are the symptoms of hyperthyroidism that are most frequently linked to it, it can also cause mood swings and, in certain situations, even worsen depression.
Thyroid hormone and brain function: The growth and operation of the brain are significantly influenced by thyroid hormones. They are necessary for the central nervous system's healthy growth and operation. Thyroid hormone fluctuations may have an effect on the neurotransmitter balance in the brain, which may have an effect on mood control.
Thyroid treatment depression symptoms: When treated, thyroid dysfunction may help some people with treatment-resistant depression by reducing their depressed symptoms. When diagnosing and treating depression in patients, medical providers must take thyroid function into account. Thyroid dysfunction can lead to depression because the thyroid gland plays a crucial role in regulating various bodily functions, including mood and emotional well-being. There are two primary thyroid conditions that can contribute to depression: hypothyroidism and hyperthyroidism.
Hypothyroidism (Underactive Thyroid):
Hypothyroidism occurs when the thyroid gland doesn't produce enough thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3).Thyroid hormones play a role in regulating metabolism and brain function, and they influence the production and function of neurotransmitters, such as serotonin and norepinephrine, which are associated with mood regulation.In hypothyroidism, the decreased levels of thyroid hormones can result in a slower metabolism, fatigue, weight gain, and a range of physical symptoms. These physical symptoms can contribute to low self-esteem and feelings of hopelessness, which are common features of depression.Additionally, the altered neurotransmitter levels can directly impact mood and contribute to depressive symptoms.
Hyperthyroidism (Overactive Thyroid):
Hyperthyroidism, on the other hand, is when the thyroid gland produces excessive thyroid hormones.
In hyperthyroidism, individuals may experience symptoms like anxiety, restlessness, irritability, and rapid heart rate, which can mimic the symptoms of anxiety and panic disorders.These anxiety-related symptoms can be accompanied by emotional disturbances, including mood swings and emotional instability, which can contribute to or exacerbate depressive symptoms.
It's important to note that while thyroid dysfunction can contribute to depression, it is not the sole cause of depression. Depression is a complex mental health condition influenced by various factors, including genetics, environmental factors, and life experiences. Thyroid dysfunction is just one potential factor among many that can contribute to depressive symptoms. If you suspect that your thyroid function may be related to your depressive symptoms, it's crucial to seek medical evaluation and treatment. Thyroid conditions can often be effectively managed with medication or other medical interventions, which can help alleviate both the physical and emotional symptoms associated with thyroid dysfunction. Additionally, addressing any underlying depression with psychotherapy and/or medication may also be necessary for a comprehensive treatment approach
AIMS:
The aim of the study is to determine the depression due to thyroid dysfunction.
OBJECTIVES:
- To identify the individuals suffering from depression due to thyroid dysfunction.
- To prevent depression and to give treatment for thyroid dysfunction.
- To identify the relation between the depression and thyroid.
Literature Review:
- Manuel R. Blum; Liselotte W. Wijsman; Vanessa S. Virgini; Douglas C. Bauer; Wendy P.J. den Elzen;J. Wouter Jukema; Brendan M. Buckley; Anton J.M. de Craen; Patricia M. Kearney; David J. Stott; Jacobjin Gussekloo; Rudi G.J. Westendorp; Simon P. Mooijaart (2016). Subclinical Thyroid Dysfunction and Depressive Symptoms among the Elderly: A Prospective Cohort Study. Conclusions: In this largest prospective study on the association of persistent subclinical thyroid dysfunction and depression, subclinical hypothyroidism was not associated with increased depressive symptoms among older adults at high cardiovascular risk. Persistent subclinical hyperthyroidism might be associated with increased depressive symptoms which requires confirmation in a larger prospective study.
- B .Harris ,S. Othman, J.A Davies, G. J. Weppner, C.J Richards, R. G. Newcombe .H .Lazarus, R.Hall, A .B. Parkers. Increased risk of depression with hypothyroidim Conclusion : Depressive symptoms are associated with positive thyroid antibody status in postpartum period.
- Till Ittermann, Henry Völzke , Sebastian E. Baumeister, Katja Appel & Hans J. Grabe Social psychiatry and psychiatric epidemiology 2015. Conclusion: Our results substantiate evidence that diagnosed untreated hypothyroidism is associated with depression and anxiety, and that diagnosed untreated hyperthyroidism is associated with depression.
- B.Harris,S. Othman, J.A Davies, G.J.Weppner, C.J Richards, R.G.Newcombe .H.Lazarus, R.Hall, A.B.Parkers. Increased risk of depression with hypothyroidim Conclusion : Depressive symptoms are associated with positive thyroid antibody status in postpartum period
- Osvaldo P. Almeida M.D., Ph.D., F.R.A.N.Z.C.P. a b c, Helman Alfonso M.D., Ph.D. a b, Leon Flicker M.B.B.S., Ph.D., F.R.A.C.P. a d e, Graeme Hankey M.B.B.S., M.D., F.R.A.C.P., F.R.C.P. d f, S.A. Paul Chubb B.Sc., Ph.D. g, Bu B. Yeap M.B.B.S., Ph.D. d h Community-dwelling sample of 3,932 men age 69 to 87 free of overt thyroid disease. Conclusion : Subclinical thyroid disease is not associated with prevalent or incident depression in older men. These findings do not support the routine screening of subclinical thyroid dysfunction among older adults with depression.
- A study by Engum et al.(2002) found that individuals with subclinical hypothyroidism were at an increased risk od developing depressive symptoms . increased risk of hypothyroidism. Conclusion: Prospective studies consistently show that individuals with hypothyroidism have a higher risk of developing depression
- Rajiv Radhakrishnan,* Sam Calvin,** Jyotin Kshitiz Singh, Binston Thomas, and Krishnamachari Srinivasan. Thyroid dysfunction in major psychiatric disorders in a hospital based sample. Conclusion : Abnormal thyroid hormonal status in general, and presence of hypothyroidism and hyperthyroidism, in particular were seen in 29.3, 25.17 and 4.08 per cent patients with schizophrenia spectrum disorders, respectively. These were comparable to the rates in patients with mood disorders (23.24, 21.62 and 1.62%, respectively). Eleven of the 18 patients with antiTPO positivity had a schizophrenia-spectrum disorder. There were no gender differences. Thyroid dysfunction was present in patients with schizophrenia-spectrum disorder as well as mood disorders. Autoimmune thyroid disease was more commonly seen in patients with schizophrenia-spectrum disorders compared to mood disorders. The findings reiterate the relevance of screening patients with schizophrenia-spectrum disorders for abnormal thyroid hormonal status.
- Michael Bauer (2012). The link between thyroid function and depression. Conclusion: Clinical investigators have long recognized the link between thyroid and depression. While patients with hypothyroidism commonly manifest features of depression, hyperthyroidism presents with a wider spectrum of neuropsychiatric symptoms including both depression and anxiety. On the other hand, most of the patients with primary depression have normal thyroid function. The mechanisms underlying the interaction between thyroid function and depression remain to be clarified and a causal relationship between the two cannot be established yet. A possible role for thyroid autoimmunity in the pathogenesis of depression can be elucidated. Screening patients presenting with depression for thyroid dysfunction seems reasonable particularly those with refractory symptoms. However, the use of thyroid hormones as an adjunct therapy to antidepressants in the absence of subclinical or clinical hypothyroidism should be further investigated. In addition, specifying a particular patient population that might benefit from this combination as determined by individual genetic variants should be addressed. The continuing research in the biochemical, genetic, and neuroimaging fields seems most promising in providing a deeper understanding of the thyroid-depression interactions.
- Dr. Sasi kala, Attar Monisha , Challa Ganesh babu (2023) A Prospective study on depression due to thyroid dysfunction .Conclusion : When the thyroid gland does not produce enough thyroid hormones, hypothyroidism results. Feelings of depression and low mood can be exacerbated by symptoms of this condition, which include fatigue, weight gain, cold intolerance, and a general slowing of bodily functions. Depression symptoms are more likely to manifest in people with hypothyroidism. Low energy, depression, cognitive decline, and a loss of interest in once-enjoyed activities are some of these symptoms. The opposite of hypothyroidism is hyperthyroidism, a condition in which the thyroid gland overproduces thyroid hormones. Symptoms such as anxiety, agitation, fast heartbeat, and weight loss may result from this.Anxiety, emotional instability, and mood swings are sometimes experienced by people with hyperthyroidism, and these symptoms can resemble those of depression.
MATERIALS AND METHODS
1.Study design:An observational study is going to be conducted on depression due to thyroid dysfunction from a period of September 2023 to February 2024
2.Study area:This study will conduct at Narayana Medical college and hospital.
3.Study population:On 200 patients
4.Study period:From September 2023to February 2024.
5.Inclusion and Exclusion criteria:
Inclusion criteria:
- The patient with depression with past history of thyroid dysfunction.
- Only adults are included.
Exclusion criteria
- The pediatric children are not included.
- Pregnant women is not considered.
- Patient with depression and without thyroid dysfunction.
Estimation of sample size:
On 200 patients.
Sampling Method and Recruitment Process:A random sampling technique will be used to select study participants. All Patients with depression and thyroid dysfunction are selected for the evaluation.
Recruitment of study participants in the OP and IP of psychiatric department of the hospital after taking consent from the patients attenders.
Data collection and procedure +: The data is going to be collected through by face to face interviews using semi structured questionnaires and [followed up by through telecommunication].
Data Management:All questionnaires and each follow up data were stored through the study and accessed only by the researcher so as to ensure confidently and to avoid data loss. After data collected, a double entry of the same data was done for accuracy purposes. Data was entered using Microsoft Excel. The data was stored in a secured computer Data cleaning was done whereby missing values, extreme values and inconsistencies were identified and corrected After cleaning the data were exported to SPSS software version 20.0Coding and verification of the data was done for easy manipulation, analysis and presentation. Data was presented using tables and graphs showing frequency distribution for independent and dependent variables.
Data analysis:Quantitative data analysis was done using SPSS software version 20.0
Ethical consideration:The study was approved and permission to conduct the study at Narayana Medical College and Hospital was obtained from at Narayana Medical College and Hospital Administration. The details of the study were explained to each study participants. to ensure confidentiality of participants, information, anonymous typing was used whereby the name of the participants and any identifiers of the participants were not written on the questionnaire, and also to keep privacy, they were interviewed alone
RESULTS:
The prospective observational study was conducted in department of Psychiatry for 6 months in tertiary care teaching hospital i.e Narayana Medical Collage, Hospital .Nellore. The study was conducted in 200 patients who were suffering with Depression due to Thyroid dysfunction.The subjects were recruited based on inclusion and exclusion criteria .this chapter present the analysis of study findings .It is organized as follows descriptive .study of the variables .The results are represented in tabular and graphical forms.
The data of subjects collected were studied results were analyzed to meet the objectives of the stud.


 Attar monisha*
Attar monisha*
 Challa Ganesh babu
Challa Ganesh babu
 P.sasikala
P.sasikala




 10.5281/zenodo.14604394
10.5281/zenodo.14604394