Abstract
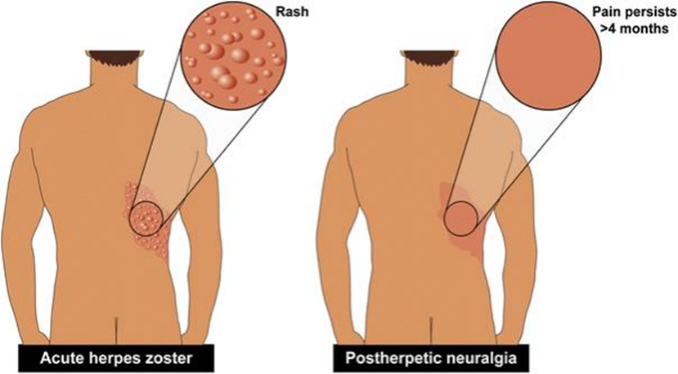
Postherpetic neuralgia has been variably Defined but is generally understood to pain that persists For longer than a few months after an attack of herpes Zoster. Pain persists for years in approximately 10 % of Those afflicted with acute herpes zoster. The likelihood of Postherpetic neuralgia increases with older age, severity Of the zoster, trigeminal location, and other factors. Postherpetic neuralgia is a neuropathic pain and treatment Usually involves sequential trials of topical and systemic Drugs; a variety of other therapies may be considered in Refractory cases. A new topical capsaicin 8 % patch has Been approved for this indication based on the positive Studies in patients with non-trigeminal postherpetic neuralgia. Experience with the use of the capsaicin 8 % patch For trigeminal distribution neuralgia is lacking. We report a Case of trigeminal postherpetic neuralgia which was safely and effectively treated with capsaicin 8 % patch
Keywords
capsaicinoids, neuropathic pain , shingles infection
Introduction
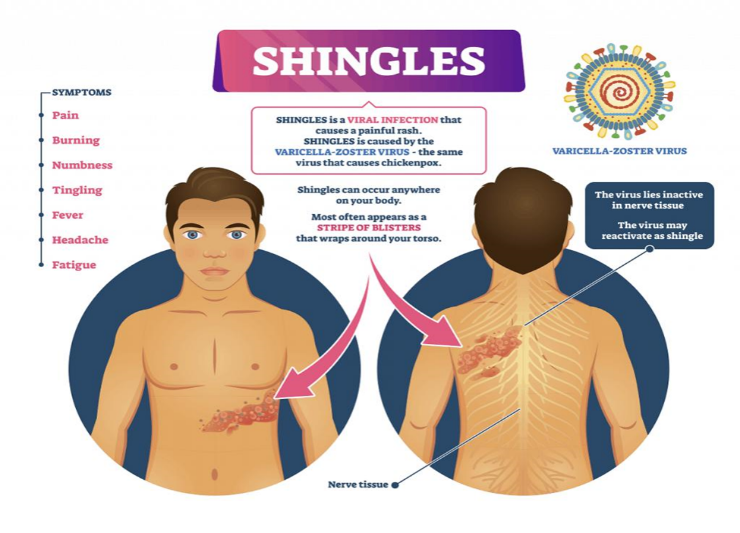
Postherpetic neuralgia (PHN) is the persistence of pain after the disappearance of the rash caused by the herpes zoster virus. The definition of PHN has been controversial, ranging from pain persisting after the healing of rash to pain that continues beyond a period that varies between 1 and 6 months. Risk factors for PHN include older age, immunosuppression, female gender, presence of prodrome, greater rash severity, and greater acute pain[1]. The thoracic dermatomes are most commonly affected, followed by the region innervated by the ophthalmic division of the trigeminal nerve, particularly that supplied by the frontal branch of V1. Antidepressants, gabapentin, pregabalin, opioids, and topical lidocaine have been shown to be efficacious in randomized controlled studies and many other drug therapies, interventional approaches, and psychological or rehabilitative treatments are tried empirically in those with persistent pain[2].
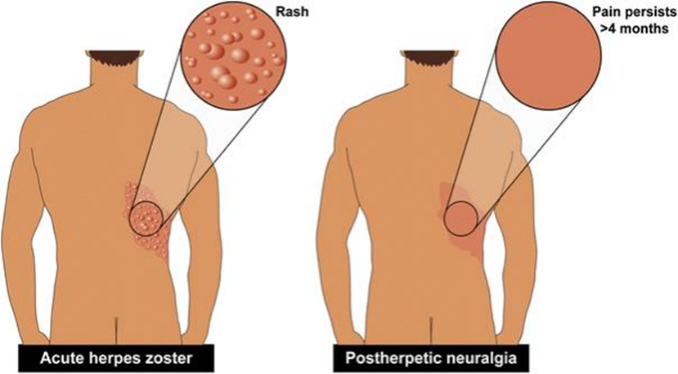
Fig: Post-herpetic Disease Condition
Low concentration topical capsaicin has been used for decades as a treatment for PHN, with equivocal results. In recent years, a high concentration (8 %) capsaicin patch has been developed, and approved for PHN based on two randomized controlled studies demonstrating the efficacy and safety of a 1-h application for PHN in non-trigeminal dermatomal distributions[3]. This treatment may reduce pain for many months and the controlled trials suggest that a typical responder will experience improvement for approximately 3 months.
Pathophysiology
The pathophysiology of PHN involves disturbances within the central and peripheral nervous systems (PNS). During the AHZ episode the dormant virus becomes activated, replicates, and propagates along the affected nerve, ultimately triggering an inflammatory immune response capable of damaging peripheral and central neurons[4]. Newly synthesized viral particles undergo axonal transport along the central and distal axons of all types of sensory neurons. This causes generalized necrosis and cell death in the skin (and sometimes in the CNS) and within the nerve, root, and ganglion. Damaged, the peripheral nerves lose the ability to inhibit nociception pain signals. This lowers the threshold for nociceptive pain activation and produces spontaneous ectopic discharges. The end result generates disproportionate pain with non-painful stimuli, a phenomenon known as peripheral sensitization[5]. HZV-induced nerve inflammation also impairs the descending inhibitory pain pathways, secondary to compromise of the dorsal horns, and leads to central sensitization. At the cellular level, PHN upregulates the receptors typically associated with pain, such as the transient receptor potential vanilloid 1 (TRPV1) , as well as an increase in the proportion of voltage-gated sodium channels and potassium voltage-gated channels. There is also evidence of loss of ?-amino butyric acid inhibitory interneurons at the dorsal horn in addition to loss of descending inhibition. Watson et al. Compared autopsy tissue from patients with and without PHN after shingles and found that patients with PHN had marked degeneration of their spinal cord dorsal horns. However, it remains unknown whether this dorsal horn atrophy is caused by direct infection of the spinal cord or by trans-synaptic degeneration. Although there is predilection for involvement of sensory ganglia and nerves, motor deficits may occur from the spread of the infection and inflammation to the anterior horn of the spinal cord[6]. Motor neuron axons or cell bodies often undergo degeneration due to the spread of inflammatory cells and molecules from nearby infected somatosensory cells, and some patients develop signs of motor compromise as well as pain.
Epidemiology
In a survey conducted between 1988 and 1994 in the US, over 99% of adults aged ?40 years had serologic evidence of prior VZV infection and are therefore at risk of developing HZ[10]. Approximately 1 million cases of HZ occur annually in the US, and one in every three persons develops HZ during their lifetime. It is estimated that 5%–20% of those with HZ go on to develop PHN. The frequency and severity of PHN increase with advancing age, occurring in 20% of people aged 60–65 years who have had acute HZ, and in more than 30% of people aged >80 years[7]. In addition to age, risk factors for developing PHN after HZ include the presence of a prodrome (defined as pain and/or abnormal sensations before rash onset), severe rash (defined as >50 lesions: papules, vesicles, or crusted vesicles), and severe pain during the acute phase[8].
Diagnosis of PHN
A history of HZ and the nature of the pain are critical parameters of a PHN diagnosis. Thus, obtaining a detailed medical history and including symptoms and vaccination history are very important, as is performing a careful physical examination with a focus on qualifying the pain and its impact on daily life[40]. Areas previously affected by HZ may show evidence of cutaneous scarring, and the site of the pain should be inspected for rash, color changes, and edema[9]. Areas of sensory abnormalities, including allodynia (painful response to normally innocuous stimuli), hyperalgesia (heightened pain response), or dysesthesia (unpleasant and abnormal sensation), in the affected area should be assessed for sensitivity to touch (eg, light touch with a cotton swab or small paintbrush; pinprick with a safety pin or a wooden toothpick), for thermal response to warm or cold objects (eg, metal thermorollers), and/or for response to vibration (eg, using a 128 Hz tuning fork)[10].
Management of PHN
Approaches to PHN management include preventing HZ, and thus possibly PHN, through vaccination and/or antiviral treatment, and administering specific medications to treat PHN pain[11].
Shingles Infection
The Varicella-zoster virus (VZV) or human herpes virus 3 is the causative agent for both chickenpox/varicella and shingles/Herpes zoster (HZ). HZ represents a reactivation of VZV in the host and has gained interest because of variable clinical presentation, which is important in the differential diagnosis of diseases. Furthermore, HZ complications are potentially life threatening[12]. HZ reactivation has been reported as a possible adverse event after COVID-19 vaccination. Treatment options and prevention by vaccination are of clinical importance. HZ can present with different clinical manifestations, some with higher risk of complications. The literature related to HZ continues to evolve, especially in regard to patients with comorbidities and immunocompromised patients. VZV reactivation has emerged as an important point of discussion during the COVID-19 pandemic, especially after vaccination.[13] With this background, in this review we discuss the current updates related to
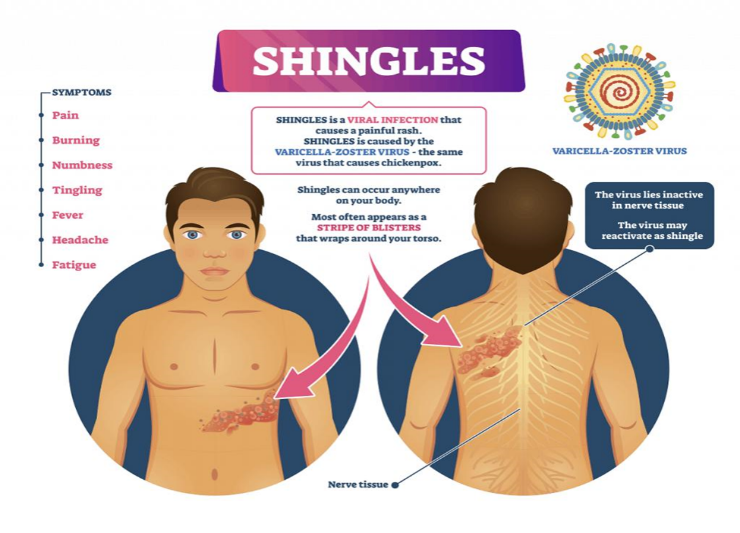
clinical presentations, complications, and management of HZ. The literature was searched through PubMed and Google Scholar to retrieve relevant published articles on HZ[14]. Clinical trials, clinical studies, review articles, systematic reviews, meta-analyses, case series, and case reports were considered for review. Keywords “Varicella-zoster virus”, “Herpes zoster”, “treatment AND Herpes zoster”, “prevention AND Herpes zoster” were used to search the articles.
Neuropathic Pain :
Neuropathic pain can be defined as a process occurring after a primary lesion or disease of the somatosensory nervous system. This condition is the result of a series of different pathological mechanisms and it is usually described based on the anatomic localization or etiology[15]. The conditions and the pathophysiological states that determine the onset of neuropathic pain mostly involved are metabolic disorders (e.g. peripheral diabetic neuropathy (PDN)), neuropathies associated with viral infections (e.g. post-herpetic neuralgia, HIV, leprosy), autoimmune disorders affecting the central nervous system (e.g. multiple sclerosis and Guillain-Barre syndrome),chemotherapy-induced peripheral neuropathies, damage to the nervous system of traumatic origin (e.g. spinal cord injury (SCI) and amputation), inflammatory disorders, hereditary neuropathies, and channelopathies[16]. Among the signs and the symptoms connected to the presence of neuropathic pain are allodynia (pain due to a stimulus that does not normally provoke pain), hyperalgesia (an increase in the perception of pain generated by a stimulus that causes Pain), and paresthesia (a condition that determines the perception of anomalous sensations comparable to needle bites, tingling, itching, reduced, or even loss of sensitivity)[21]. In patients suffering from neuropathic pain, the perceived pain is usually spontaneous, manifesting itself without needing a stimulus. This pathological condition substantially affects the quality of life of patients, compromising their psychological state[17].In the global population, the incidence and prevalence of neuropathic pain are difficult to estimate due to the lack of consensus on the definition of neuropathic pain.
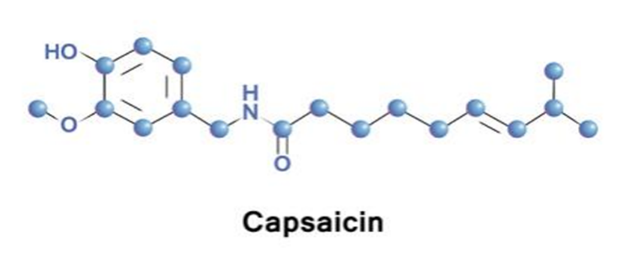
Capsaicin used in Treatment of Postherpetic Disease
Capsaicin 0.075% cream and 8% patch formulations have shown modest efficacy as monotherapy in patients with PHN. According to a 2009 Cochrane review, the NNT for any pain relief with capsaicin 0.075% cream in patients with PHN or diabetic neuropathy[18]. However, cream formulations deliver low capsaicin concentrations and must be applied 3 or 4 times daily. In contrast, capsaicin 8% patch delivers a high concentration of capsaicin in a single 60 minute application after application of a local anesthetic, with the result that improved compliance and more efficient drug delivery may translate into improved efficacy for the patch compared with cream formulations. The NeuPSIG guidelines list capsaicin creams as third-line therapy, citing inconsistent clinical trial data supporting its efficacy in patients with PHN. Only the EFNS guidelines discuss both capsaicin cream and the capsaicin 8% patch, citing clinical trial data for the capsaicin 8% patch published after the appearance of the AAN and NeuPSIG guidelines[19].
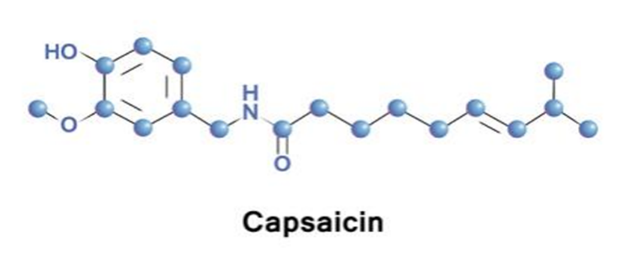
Topical application of capsaicin results in very little systemic distribution even with the high concentration capsaicin 8% patch, making systemic AEs and drug interactions unlikely. Application-site reactions are the most frequent AE with capsaicin creams and have been reported in up to 96% of patients who applied the capsaicin 8% patch[20]. Mostly these reactions consist of application-site burning and transient dermal irritation that resolves in several days. Pain during treatment is a significant problem (and the leading cause of treatment discontinuation) with capsaicin creams, which need to be applied multiple times daily. A topical anesthetic is recommended when applying the capsaicin 8% patch. The EFNS guidelines observe that the long-term effects on repeat treatment on the normal sensitivity of nerves to both benign and noxious stimuli remain to be determined.
- Morphology
Chilli (Capsicum annuum L.) An herbaceous or semi-woody, annual plant during early stage of growth but becomes woody later on. The old branches become brittle with age and are easily broken. Straight, woody stems and the leaves are ovate, tapering to a sharp point, measuring up to 15 cm, dark green on the upper surface and pale green on the lower surface[21]. The leaves are simple, alternate, exstipulate, elliptic, lanceolate, and glabrous. Leaf area per plant and leaf length varies from 1000-3000sq.cm and 0.5-2.5 cm, respectively. Chilli plant possess strong tap root which is usually broken or arrested during transplanting, resulting in the development of profusely branched laterals as much as 1 m long. The entire root system remains restricted to the upper soil layer of 30 cm depth but more active feeding roots are found up to 10 cm depth from the base of the plant.

- Extraction of capsaicin
Capsicum annuum L. or chili is a well-known plant found through the world. Its fruit is commonly used as a spice and added in various types of cuisines and is also used in traditional medicine. The fruit of Capsicum species or hot peppers contains a group of compounds that give them their characteristic pungent flavour[22]. These compounds are called capsaicinoids. The major component of this group is capsaicin. Capsaicin and its related compounds are used in folk medicine for different purposes, such as to relieve pain and to treat arthritis. There are many organic liquids that are used as solvents to extract chemical compounds from plants and other organisms. For extraction of capsaicin from chili, several studies have been conducted using various solvents. These include methanol-water, methanol-surfactant, methanol-water-surfactant, and water-surfactant solutions. Quantification of capsaicin in the extracts were determined by UV-visible spectrophotometry method. This method has an obvious limitation since the extracts not only contained the desired compound capsaicin but also other phytochemicals extractable under the experimental conditions, which may contribute to the absorbance. However, the method is widely used as it is robust, convenient, and cost-effective and gives a reasonable estimate of the desired compound. The method has also been used for the quantification of capsaicin. With this background in view, the current work was designed with the objectives to evaluate the effectiveness of different solvents for extraction of capsaicin from chili and to investigate the effect of anionic, cationic and non-ionic surfactants on the extraction efficiency of the solvents with significant effectiveness[23].
- Mechanism of action
The broad traditional usage of chili has prompted the identification of capsaicin as the main active component of a variety of chili peppers such as habaneros and jalapeños. Capsaicin is responsible for causing the ‘hot’ and sharp pungent sensation[24]. Those properties have been suggested to act through counter-irritation, which results in analgesic effects. Modern usage of capsaicin focuses on the treatment of various types of pain . In fact, capsaicin has been studied clinically as a topical treatment for the pain of rheumatoid and osteoarthritis , psoriasis, diabetic neuropathy, and postherpetic neuralgia[35]. However, the efficacy of capsaicin in the treatment of these chronic pain disorders is still elusive. In order to have a better understanding of the various action of capsaicin, studies have focused on the mechanism of capsaicin in pain induction. It is known as a selective TRPV1 receptors ligand. The burning sensation is triggered upon the binding of capsaicin to the receptors. It is believed that the analgesic effect of capsaicin is due to its ability to cause reversible desensitization or DE functionalization, where the TRPV1 containing sensory axons become unresponsive to stimuli during the long-lasting refractory period As a result, after repeated exposure to capsaicin, pain transmission is prevented and the pain response is reduced irritant components. This feature of capsaicin has been exploited for therapeutic use for many years. Other than that, its ability to cause reversible nerve-fiber degeneration also contributes to the analgesic effect. Conventionally, topical capsaicin has been used in pain management in numerous neuropathic pain conditions. FDA, the Qutenza patch, a pure, synthetic capsaicin-containing prescription drug, was approved by the Food and Drug Administration (FDA) for long-term pain relief for PHN patients. In spite of that, its safety has been much debated. This is mainly because capsaicin is associated with some severe side effects such as capsaicin-induced dermal pain and contact dermatitis (human hand)[25]. Topical capsaicin products such as Qutenza may cause a significant rise in blood pressure, necessitating the need for blood-pressure monitoring by health care professionals. Emerging evidence has also suggested that long-term application of topical capsaicin may be harmful.

CONCLUSION
Capsaicin, the main component in chili peppers, has immense ethnopharmacological potential, and has served as one of the main adjunctive treatments for neuropathic pain such as PHN. The current review aimed to compile and investigate the efficacy and safety of topical capsaicin in management of chronic nipain caused by PHN. Based on a literature search, all the six included studies suggest that topical capsaicin is efficacious but at the same time is associated with a higher incidence of side effects. This prompted the need for a meta-analysis study. Based on the analysis, five of the included studies indicated the treatment with capsaicin has better efficacy compared to a vehicle-controlled placebo. However, the results of two studies involving 298 out of the 1415 total pooled population are not statistically significant. Unfortunately, the answer to the research question remains inconclusive. Therefore, it is still unclear whether or not topical capsaicin should be used as a first-line treatment. Further evidence is required to determine the risk-benefit ratio and support the use of capsaicin as a first-line treatment.
REFERENCE
-
-
-
- Kost RG, Straus SE (1996) Postherpetic neuralgia-pathogenesis, Treatment, and prevention. N Engl J Med 335:32–42
- Cunningham AL, Dworkin RH (2000) The management of post-herpetic neuralgia. BMJ 321:778–779
- Nagasako EM, Johnson RW, Griffin DR et al (2002) Rash severity in herpes zoster: correlates and relationship to postherpetic neuralgia. J Am Acad Dermatol 46:834–839
- Goh CL, Khoo L (1997) A retrospective study of the clinical presentation and outcome of herpes zoster in a tertiary dermatology outpatient referral clinic. Int J Dermatol 36:667–672
- Dworkin RH, Johnson RW, Breuer J et al (2007) Recommendations for the management of herpes zoster. Clinical Infect Disease 44:S1–S26
- Edelsberg JS, Lord C, Oster G (2011) Systematic review and meta-analysis of efficacy, safety, and tolerability data from randomized controlled trials of drugs used to treat postherpetic neuralgia. Ann Pharmacotherapy 45:1483–1490
- Haythornthwaite JA, Benrud-Larson LM (2001) Psychological assessment and treatment of patients with neuropathic pain. Curr Pain Headache Rep 5:124–129
- Wu CL, Raja SN (2008) An update on the treatment of postherpetic neuralgia. J Pain 9:S19–S30
- Woolf CJ, Mannion RJ. Neuropathic pain: etiology, symptoms, mechanisms, and management. Lancet. 1999;353(9168):1959–1964.
- Gagliardi AM, Gomes Silva BN, Torloni MR, Soares BG. Vaccines for preventing herpes zoster in older adults [review]. Cochrane Database Syst Rev. 2012;10:CD008858.
- Dworkin RH, O’Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132(3):237–251.
- Centre for Clinical Practice at NICE (UK) – National Institute for Health and Care Excellence: Clinical Guidelines. Neuropathic Pain: The Pharmacological Management of Neuropathic Pain in Adults in Non-specialist Settings. London: National Institute for Health and Care Excellence, UK; 2013.
- Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85(3 Suppl):S3–14.
- Neurontin® (gabapentin) [package insert]. New York, NY: Parke-Davis Division of Pfizer, Inc.; 2015.
- Kilgore PE, Kruszon-Moran D, Seward JF, et al. Varicella in Americans from NHANES III: implications for control through routine immunization. J Med Virol. 2003;70(Suppl 1):S111–S118.
- Harpaz R, Ortega-Sanchez IR, Seward JF; Advisory Committee on Immunization Practices (ACIP) Centers for Disease Control and Prevention (CDC). Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008;57(RR-5):1–30.
- Fashner J, Bell AL. Herpes zoster and postherpetic neuralgia: prevention and management. Am Fam Physician. 2011;83(12):1432–1437.
- Gharibo C, Kim C. Neuropathic pain of postherpetic neuralgia. Pain Med News. 2011;9:84–92.
- Forbes HJ, Thomas SL, Smeeth L, Clayton T, Farmer R, Bhaskaran K, Langan SM. A systematic review and meta-analysis of risk factors for postherpetic neuralgia. Pain. 2016;157(1):30–54.
- Backonja MM, Attal N, Baron R, et al. Value of quantitative sensory testing in neurological and pain disorders: NeuPSIG consensus. Pain. 2013;154(9):1807–1819.
- Li Puma, D.D.; Marcocci, M.E.; Lazzarino, G.; De Chiara, G.; Tavazzi, B.; Palamara, A.T.; Piacentini, R.; Grassi, C. Ca2+-dependent release of ATP from astrocytes affects herpes simplex virus type 1 infection of neurons. Glia 2021, 69, 201–215.
- Colloca L, Ludman T, Bouhassira D, et al. (2017) Neuropathic pain. Nature Reviews Disease Primers 3: 17002.
- Derry S, Lloyd R, Moore RA, McQuay HJ. Topical capsaicin for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2009;4:CD007393.
- US Food and Drug Administration. FDA approves new drug treatment for long-term pain relief after shingles attacks. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2009/ucm191003.ht Accessed June 30, 2011.
- FDA (2009). FDA Approves New Drug Treatment for Long-Term Pain Relief After Shingles Attacks [Online]. Silver Spring, MD: U S Food and Drug Administration (FDA)


 Umesh Jadhav *
Umesh Jadhav *
 Nikam H. M
Nikam H. M


 10.5281/zenodo.14608460
10.5281/zenodo.14608460