Abstract
Tuberculosis (TB) is a contagious and potentially fatal infectious disease primarily caused by Mycobacterium tuberculosis, most commonly affecting the lungs, but it can also involve other organs (extrapulmonary TB). TB remains a major global health concern, with an estimated 10 million cases and 1.5 million deaths annually. The disease is transmitted through airborne droplets when an infected person coughs or sneezes. Symptoms of active TB include persistent cough, chest pain, fever, night sweats, weight loss, and fatigue. TB can be latent, where the bacteria remain dormant in the body without causing symptoms, or active, where it leads to disease and is contagious. Diagnosis is typically confirmed through sputum smear microscopy, chest X-ray, and molecular tests like PCR. Treatment involves a combination of antibiotics, including isoniazid, rifampin, pyrazinamide, and ethambutol, for a duration of 6-12 months. Drug-resistant TB, including multi-drug resistant (MDR) and extensively drug-resistant (XDR) strains, presents a significant challenge to treatment and public health. While conventional therapies are critical, there is growing interest in adjunctive treatments, including herbal remedies, to support the immune system and alleviate symptoms. However, such therapies should never replace standard drug regimens. Effective control of TB requires early diagnosis, adherence to treatment, and continued efforts in public health strategies, including vaccination, to reduce transmission and the burden of the disease globally.
Keywords
Ethiopia; Medicinal plants; Traditional; Treatments; Tuberculosis.
Introduction
Tuberculosis (TB) is a contagious bacterial infection primarily affecting the lungs, though it can spread to other parts of the body such as the kidneys, spine, and brain. It is caused by Mycobacterium tuberculosis, a slow-growing bacterium that spreads through the air when an infected person coughs or sneezes. TB remains one of the world’s leading infectious diseases, particularly in developing countries, where it is often linked with poverty, malnutrition, and weakened immune systems, such as those in people living with HIV/AIDS. The disease typically progresses slowly, with symptoms that may include persistent coughing, chest pain, weight loss, fever, and night sweats. In some cases, TB can remain latent in the body without symptoms, but it can become active if the immune system weakens. TB is treatable with a combination of antibiotics, though the rise of drug-resistant strains has made treatment more challenging. Early diagnosis and adherence to the full course of treatment are crucial to prevent the spread of the disease and reduce the risk of complications. Public health efforts, including vaccination with the Bacillus Calmette Guérin (BCG) vaccine and improved healthcare access, have helped control TB in many parts of the world, though it remains a global health concern.
WHAT IS TUBERCULOSIS (T.B):
Tuberculosis (TB) is a contagious bacterial infection primarily caused by Mycobacterium tuberculosis. While it most commonly affects the lungs (pulmonary TB), TB can also affect other parts of the body, such as the kidneys, spine, brain, and lymph nodes (extrapulmonary TB).
TB is spread through the air when an infected person coughs, sneezes, or talks, releasing tiny droplets containing the bacteria into the air. People who breathe in these droplets can become infected. However, not everyone who is exposed to TB will develop active disease. In many cases, the bacteria can remain dormant in the body (latent TB) without causing symptoms. If the immune system weakens, latent TB can progress to active TB.
PATHOPHYSIOLOGY:
The pathophysiology of tuberculosis (TB) involves complex interactions between the Mycobacterium tuberculosis bacteria and the host’s immune system. TB primarily affects the lungs (pulmonary TB) but can spread to other organs (extrapulmonary TB). The development of TB and the progression of the disease depend on the immune response to the bacteria, the ability of M. tuberculosis to evade immune defenses, and factors such as host immunity, genetic predisposition, and the presence of comorbid conditions (e.g., HIV).
1. Entry and Initial Infection
• Transmission: TB is transmitted via airborne droplets when an infected person coughs, sneezes, or talks. These droplets contain M. tuberculosis, which can be inhaled by a susceptible individual.
• Infection: The bacteria initially enter the lungs and are carried into the alveoli (air sacs) by inspired air. The alveolar macrophages, which are the first line of defense against pathogens, attempt to engulf and kill the bacteria.
2. Immune Response and Granuloma Formation
• Macrophage Response: Mycobacterium tuberculosis has evolved to survive inside macrophages. It can inhibit the normal killing mechanisms of the macrophages, such as the fusion of phagosomes with lysosomes. This allows the bacteria to multiply within the macrophages.
• T-cell Activation: The body’s immune system recognizes the infection and activates CD4+ T-helper cells, which release cytokines (e.g., interferon-gamma). This leads to the activation of macrophages and other immune cells.
• Granuloma Formation: In an attempt to control the infection, the immune system forms a granuloma. A granuloma is a collection of immune cells, primarily macrophages, surrounded by lymphocytes. This structure walls off the bacteria and limits their spread. Central areas of the granuloma may undergo caseous necrosis (a type of tissue death characterized by a cheese-like appearance), which is a hallmark of TB.
3. Latent TB Infection (LTBI)
• Dormancy: In most cases, the immune system can control the infection, but not eliminate it. The bacteria enter a dormant or latent state within the granulomas. In this latent form, TB remains asymptomatic, and the person is not contagious.
• Immunocompetence: Latent TB is controlled by a strong immune response, with low-grade inflammation and immune surveillance keeping the bacteria in check. Latent TB can persist for years without causing symptoms.
4. Reactivation of TB (Active Disease)
• Immunosuppression: If the immune system becomes weakened (due to factors like HIV infection, malnutrition, diabetes, or immunosuppressive medications), dormant bacteria can reactivate and begin multiplying again. This leads to active TB disease.
• Lung Damage: As the bacteria multiply, they can cause tissue destruction, particularly in the lungs. The caseous material may liquefy, leading to the formation of cavities in the lung tissue. These cavities provide an environment where the bacteria can thrive and spread.
• Cough and Spread: In active TB, the infection causes a persistent cough, often with blood-tinged sputum. This allows the bacteria to be expelled and transmitted to others through airborne droplets.
5. Extrapulmonary TB
• Spread to Other Organs: In some cases, the bacteria spread through the bloodstream (hematogenous spread) to other parts of the body, leading to extrapulmonary TB. This can involve organs such as the liver, kidneys, bones, brain, and lymph nodes. The immune response to extrapulmonary TB can vary depending on the organ affected.
• Tuberculous Meningitis: When TB affects the brain, it can cause tuberculous meningitis, which leads to symptoms such as headache, fever, neck stiffness, and confusion.
6. Pathogenesis in Drug-Resistant TB
• Drug Resistance: When M. tuberculosis develops resistance to one or more of the first-line anti-TB drugs (e.g., isoniazid or rifampin), the bacteria can persist and continue to multiply. Multi-drug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB) are particularly difficult to treat, leading to prolonged illness and a higher risk of death. Resistance arises due to mutations in the bacteria’s DNA, often exacerbated by incomplete treatment or poor adherence to therapy.
SYMPTOMS:
The symptoms of tuberculosis (TB) can vary depending on whether the infection is latent (inactive) or active (causing disease). Active TB is contagious and can affect various organs, but most commonly, it affects the lungs (pulmonary TB). Extrapulmonary TB can affect other parts of the body, such as the kidneys, bones, brain, and lymph nodes.
Symptoms of Active Pulmonary TB (Lung TB):
1. Persistent Cough: A cough lasting more than 3 weeks, often producing mucus or blood (hemoptysis). This is one of the hallmark symptoms of active TB.
2. Chest Pain: Pain in the chest, especially when coughing or breathing deeply.
3. Fever: A low-grade fever, often occurring in the evening or night.
4. Night Sweats: Excessive sweating at night, which can soak through clothing or sheets.
5. Fatigue and Weakness: Unexplained tiredness or weakness, even with minimal activity.
6. Weight Loss: Unintentional weight loss, which can be significant over time.
7. Loss of Appetite: Reduced appetite, often accompanying weight loss.
8. Shortness of Breath: Difficulty breathing, especially with exertion, as the disease progresses and lung function is impaired.
9. Coughing Up Blood: In more severe cases, coughing may be accompanied by blood (hemoptysis).
Symptoms of Extrapulmonary TB (TB affecting organs other than the lungs):
Extrapulmonary TB can present with a wide variety of symptoms depending on the organ affected. Some common forms of extrapulmonary TB include:
1. TB of the Lymph Nodes (Scrofula):
• Swollen, painless lymph nodes, especially in the neck or under the jaw.
2. TB of the Bones and Joints:
• Pain, swelling, and stiffness in the affected joints or bones, especially the spine (known as Pott’s disease).
3. TB of the Kidneys:
• Blood in the urine (hematuria) or painful urination.
• Possible kidney failure in severe cases.
4. Tuberculous Meningitis (TB of the Brain):
• Headache, confusion, neck stiffness, vomiting, and sensitivity to light.
• This can progress to more severe neurological symptoms, including seizures and coma.
5. TB of the Heart (Pericarditis):
• Chest pain, difficulty breathing, and symptoms of heart failure due to inflammation of the heart’s lining.
6. TB of the Gastrointestinal System:
• Abdominal pain, nausea, vomiting, and unexplained weight loss, if the digestive system is involved.
7. TB of the Skin:
• Skin lesions or ulcers, particularly in cutaneous TB.
Symptoms of Latent TB:
• No Symptoms: People with latent TB do not show any signs of illness. The bacteria are dormant in the body and cannot spread to others. However, latent TB can become active, especially if the immune system weakens.
When to Seek Medical Attention:
• Persistent Cough: A cough lasting more than 3 weeks, especially if it’s accompanied by blood or sputum.
• Unexplained Weight Loss, Fever, and Night Sweats: These symptoms, especially if combined with a history of TB exposure, require medical evaluation.
• Shortness of Breath or Chest Pain: If breathing becomes difficult or chest pain is severe, it’s important to seek immediate medical help.
CAUSES:
• Primary Cause: Mycobacterium tuberculosis, a bacteria that infects the lungs and potentially other parts of the body.
• Transmission: Airborne droplets expelled by an infected person.
• Risk Factors:
• Close contact with an active TB patient.
• Weakened immune system (due to HIV, malnutrition, diabetes, etc.).
• Living in high-risk environments (overcrowded, poor ventilation).
• Living in or traveling to TB-endemic areas.
• Genetic susceptibility or underlying lung diseases.
TB is caused by an infectious bacterium, Mycobacterium tuberculosis, which is primarily spread through the air. A variety of factors, including close contact with infected individuals, weakened immune systems, and environmental conditions, contribute to the risk of contracting and developing TB. Understanding these causes and risk factors is essential for preventing and controlling the spread of TB globally.
TREATMENT:
The treatment of tuberculosis (TB) is primarily based on the use of antibiotics to kill the Mycobacterium tuberculosis bacteria. Effective treatment requires a multi-drug regimen to ensure the eradication of the bacteria, prevent the development of drug resistance, and reduce the spread of the disease. Treatment typically lasts 6 months or longer, depending on the type of TB (e.g., pulmonary, extrapulmonary, drug-resistant TB).
1. First-Line Drugs for Drug-Sensitive TB
The standard treatment for drug-sensitive TB involves a combination of four first-line antibiotics:
- Isoniazid (INH): Inhibits the synthesis of mycolic acids, essential components of the bacterial cell wall. It is one of the most effective TB drugs.
- Rifampin (RIF): Inhibits bacterial RNA polymerase, preventing bacterial transcription. It is highly effective against M. tuberculosis.
- Pyrazinamide (PZA): Works by lowering the pH inside the bacteria, disrupting their metabolism and growth. PZA is most effective in the early stages of TB treatment and inside the acidic environment of granulomas.
- Ethambutol (EMB): Inhibits the synthesis of the bacterial cell wall by interfering with the production of arabinogalactan, a component of the cell wall.
These four drugs are typically administered for 2 months during the initial phase of treatment (intensive phase). After this, Isoniazid and Rifampin are continued for 4-6 months as part of the continuation phase.
2. Standard Treatment Regimen (6-Month Course)
• Intensive Phase (First 2 months):
• Isoniazid (INH)
• Rifampin (RIF)
• Pyrazinamide (PZA)
• Ethambutol (EMB)
• Continuation Phase (Next 4-6 months):
• Isoniazid (INH)
• Rifampin (RIF)
This 6-month regimen is effective for most drug-sensitive pulmonary TB cases, with treatment monitored for side effects and adherence.
3. Treatment of Drug-Resistant TB
Drug-resistant TB occurs when the TB bacteria are resistant to one or more of the first-line drugs, either due to inadequate treatment or other factors. Multidrug-resistant TB (MDR-TB) is resistant to Isoniazid and Rifampin, the two most potent first-line drugs, while extensively drug-resistant TB (XDR-TB) is resistant to both Isoniazid and Rifampin, plus other second-line drugs.
Treatment for MDR-TB and XDR-TB: Treatment for MDR-TB and XDR-TB is more complicated and requires longer treatment with second-line drugs. These may include:
- Fluoroquinolones (e.g., Levofloxacin, Moxifloxacin)
- Injectable drugs (e.g., Amikacin, Kanamycin, Capreomycin)
- Bedaquiline: A newer drug that targets the bacterial ATP synthase, effectively killing the bacteria.
- Linezolid: An antibiotic used for resistant TB cases, especially in XDR-TB.
- Clofazimine: Often used for MDR-TB when other treatment options are limited.
The treatment course for drug-resistant TB can last 18-24 months, and success rates vary depending on factors like the extent of drug resistance, adherence to treatment, and overall health.
4. Directly Observed Therapy (DOT)
To ensure that patients complete their treatment, Directly Observed Therapy (DOT) is often used. In DOT, a healthcare worker observes the patient taking their medication daily or several times a week. This helps improve treatment adherence, reduces the risk of developing drug-resistant TB, and ensures that patients complete their full course of therapy.
5. Adjuvant and Supportive Therapies
• Vitamin B6: Isoniazid can deplete vitamin B6 (pyridoxine), so patients are often given a supplement to prevent neuropathy.
• Management of Side Effects: Regular monitoring for side effects from TB medications (such as liver toxicity from Rifampin and Isoniazid or eye toxicity from Ethambutol) is important. Blood tests may be conducted periodically to check liver function and overall health.
• Surgical Intervention: In some cases, surgery may be needed, especially if there is significant lung damage, cavitary TB, or complications like pneumothorax (collapsed lung). Surgery can also be considered for localized, drug-resistant TB when medical treatment alone is insufficient.
6. Treatment for Latent TB Infection (LTBI)
Latent TB is when a person is infected with Mycobacterium tuberculosis, but the bacteria are dormant and the person does not have active disease. Latent TB is not contagious, but it can become active later, especially in individuals with weakened immune systems. Treatment for latent TB aims to prevent the development of active TB.
• Isoniazid (INH): The most common treatment for latent TB. It is usually given for 6-9 months, although shorter regimens (e.g., 3 months of Rifapentine and Isoniazid) are also effective.
• Rifampin (RIF): As an alternative to Isoniazid, especially for those who cannot tolerate INH. Treatment is typically given for 4 months.
• Rifapentine and Isoniazid: A shorter regimen of 3 months, administered once a week under DOT, can be used for those with latent TB.
7. Vaccination: Bacillus Calmette-Guérin (BCG)
The BCG vaccine is used in many countries with high TB prevalence, primarily to prevent severe forms of TB in children, such as TB meningitis and disseminated TB. However, the BCG vaccine is not effective in preventing pulmonary TB in adults, and its use is not common in low-TB incidence countries like the U.S. and Western Europe.
8. Monitoring and Follow-Up
Regular follow-up is critical during TB treatment to assess:
• Treatment Adherence: Ensuring the patient completes the full course of therapy.
• Side Effects: Monitoring for any adverse reactions to the medications, such as liver toxicity, neuropathy, or vision changes.
• Sputum Smears and Cultures: These are used to monitor the effectiveness of treatment and determine when the patient is no longer contagious (usually after 2-3 months of treatment in drug-sensitive TB cases).
9. Prevention of TB
Preventing the spread of TB involves:
• Early Diagnosis and Treatment: Rapid detection and treatment of TB reduce transmission.
• Isolation: People with active pulmonary TB should be isolated from others, especially in the early stages of treatment.
• BCG Vaccination: In TB-endemic areas, vaccination with the BCG vaccine can help reduce severe childhood TB.
• Contact Tracing: Identifying and testing individuals who have had close contact with a TB patient to prevent outbreaks.
ERBAL TREATMENT FOR TUBERCULOSIS:
Herbal treatments for tuberculosis (TB) have been explored historically and in modern complementary medicine, often as adjuncts to conventional antibiotic therapy. While there is no definitive herbal cure for TB, some herbs have shown promise in supporting immune function, alleviating symptoms, and potentially enhancing the effects of standard TB treatment. However, these treatments should never replace antibiotics, as TB is a serious, potentially life-threatening bacterial infection that requires medical supervision.
Here’s a review of some herbs commonly studied or used in the management of TB:
- Andrographis paniculata (Kalmegh)

• Properties: Anti-inflammatory, antibacterial, and immune-boosting.
• Evidence: Some studies suggest that Andrographis can support lung health and enhance the immune response, potentially helping the body fight off infections like TB. It has shown activity against Mycobacterium tuberculosis in vitro (lab studies), although clinical evidence in TB patients is limited.
• Usage: Often used in Ayurvedic medicine to support respiratory health and treat respiratory infections.
- Garlic (Allium sativum)

• Properties: Antimicrobial, immune-enhancing, and anti-inflammatory.
• Evidence: Garlic has been studied for its antibacterial and antimicrobial properties, with some studies indicating that it can inhibit the growth of Mycobacterium tuberculosis in vitro. Garlic’s active compound, allicin, is believed to have strong antimicrobial effects.
• Usage: Raw garlic, garlic supplements, or garlic oil may be used to support immune function, although more clinical research is needed to validate its role in TB treatment.
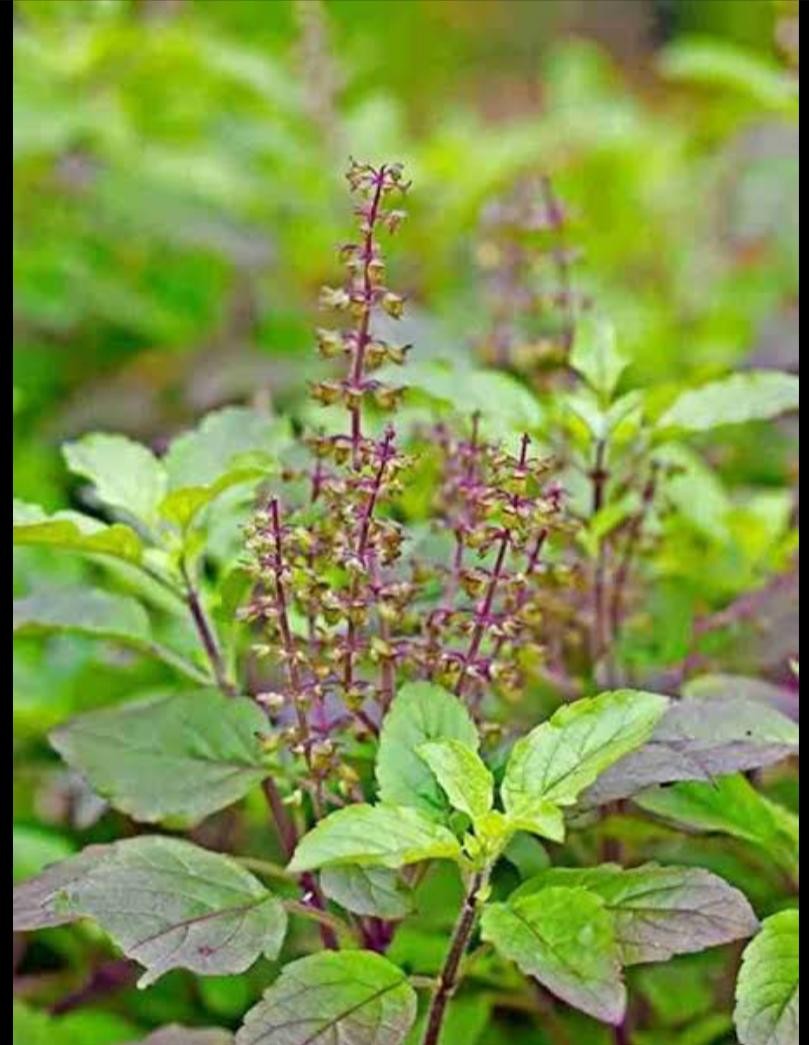
- Holy Basil (Tulsi)
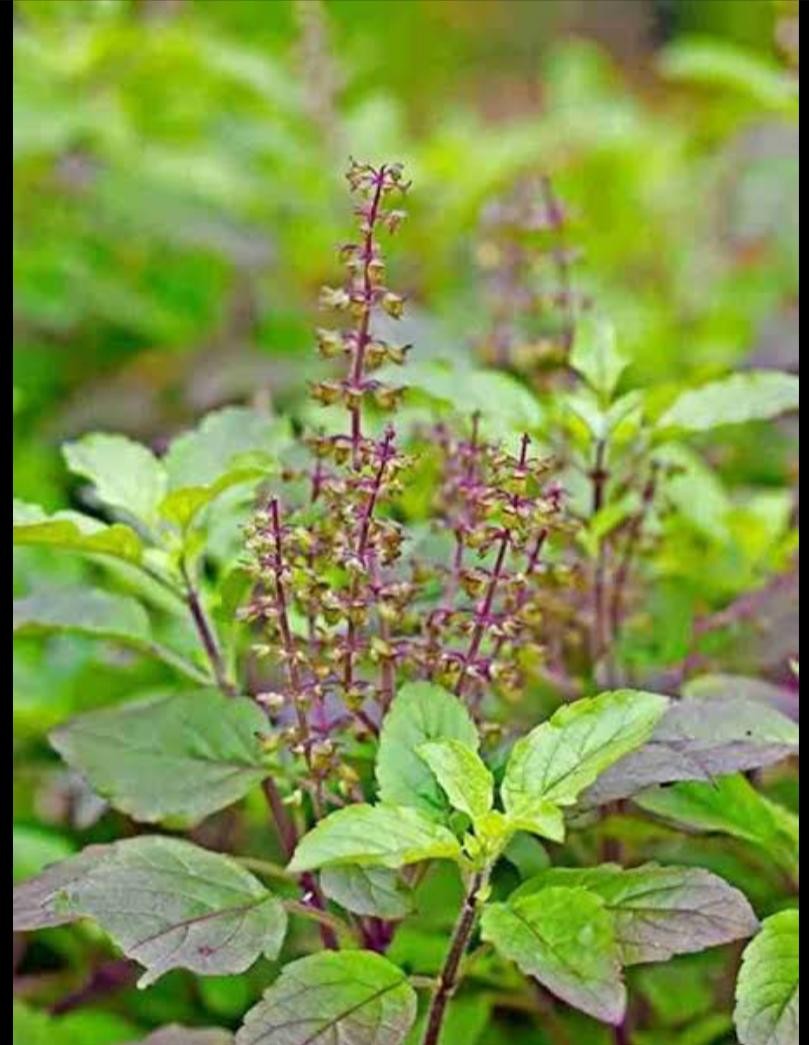
• Properties: Antibacterial, anti-inflammatory, and immune-boosting.
• Evidence: Holy Basil has traditionally been used in Ayurvedic medicine for respiratory ailments and as an immune booster. Some studies have shown that it has antimicrobial effects against a variety of pathogens, including TB, but robust clinical trials are lacking.
• Usage: Consumed as a tea, tincture, or in capsule form to potentially reduce inflammation and promote immune health.
- Astragalus (Astragalus membranaceus)

• Properties: Immune-stimulating, anti-inflammatory, and antioxidant.
• Evidence: Astragalus has been studied primarily for its effects on the immune system and its potential to enhance the body’s ability to fight infections. It is often used in Traditional Chinese Medicine (TCM) to strengthen the immune system. While there is limited direct evidence on its efficacy in TB, it may help support the body’s overall immune response, which is important in controlling TB.
• Usage: Typically taken as a supplement or in tea form.
- Licorice (Glycyrrhiza glabra)

• Properties: Anti-inflammatory, antiviral, and antibacterial.
• Evidence: Licorice has shown potential antimicrobial activity and may help soothe the respiratory tract. However, its use in TB treatment is more anecdotal, and excessive use can cause side effects such as high blood pressure or potassium depletion.
• Usage: Often used in traditional medicine for respiratory conditions, but should be used cautiously, particularly for prolonged periods or in large doses.
6. Echinacea

• Properties: Immune-enhancing, anti-inflammatory, and antimicrobial.
• Evidence: Echinacea is widely used to support immune function and fight infections. While there’s no direct evidence that Echinacea can treat TB, it may help boost the immune response in general, which could assist the body in fighting the infection.
• Usage: Commonly consumed as a tincture, capsule, or tea to boost immune health.
7. Neem (Azadirachta indica)

• Properties: Antimicrobial, anti-inflammatory, and detoxifying.
• Evidence: Neem has been used in traditional medicine for its antimicrobial properties. While some in vitro studies suggest neem has activity against Mycobacterium tuberculosis, there is limited clinical evidence to support its use in treating TB.
• Usage: Neem leaves or neem oil are used in traditional medicine, but its use for TB should be approached with caution until further evidence is available.
CONCLUSION
In Ethiopia, the number of herbal remedies is enormous and their use for TB treatment is a common practice. However, majority of them are not yet backed up by evidence generated through scientific experimentation and this warrants further experimental and clinical validations. Moreover, the efficacy, toxicity and safety tests should be initiated and this would help in the rapid identification of new anti-TB regimens, and possibly it would lead to developing more effective new plant-based drugs. This systematic review will serve as a reference for the selection of plants for developing new anti-TB regimens.
RESULT
From a total of 68 research documents that reported use of plants for treatment of TB 98 plants species belonging to 82 genera and 49 families were identified. The most frequently reported plant species belonged to family Lamiaceae (n = 8), Euphorbiaceae (n = 7), Cucurbitaceae (n = 6) and Fabaceae (n = 6). Croton macrostachyus, Allium sativum, and Myrsine Africana were the most often mentioned anti-TB medicinal plants. Shrubs (35.7%) and trees (29.6%) were reported as dominant growth forms while plant roots (31.6%) and leaves (28.6%) were frequently used plant parts for the preparations of the treatment. The most favored administration route was oral (59.1%). About 87% of the preparations were made from fresh plant materials. No experimental/clinical evidence was presented for 79.6% (78/98) of the reported plants to support their anti-mycobacterial activities. Here are some references and sources that discuss the use of herbal treatments in the context of tuberculosis (TB). These references highlight the potential roles of herbal remedies in supporting conventional TB treatment, boosting the immune system, and possibly aiding in symptom management, but they also emphasize that herbal treatments should not replace standard anti-TB medications.
REFERENCE
- Ahmad, A., & Khan, A. H. (2014). “Herbal Medicine for Tuberculosis: A Review” International Journal of Herbal Medicine, 2(6), 52-59.
- Gautam, P., & Pahwa, P. (2017). “Role of Herbal Medicine in the Treatment of Tuberculosis” Asian Journal of Pharmaceutical and Clinical Research, 10(3), 74-78.
- Srinivasan, K. (2010). “Herbal Remedies in the Treatment of Tuberculosis” Indian Journal of Traditional Knowledge, 9(1), 28-33.
- Khan, M. S., & Saleem, M. (2012). “Traditional Herbal Remedies for the Treatment of Tuberculosis” Journal of Ethnopharmacology, 143(2), 499-510.
- Bharati, S., & Joshi, R. (2015). “Potential Antimycobacterial Herbs for TB Therapy: A Review” Journal of Phytopharmacology, 4(3), 185-192.
- Subramanian, S., & Nair, A. G. (2018). “Herbal and Natural Compounds for Tuberculosis: A Comprehensive Review” Indian Journal of Natural Products and Resources, 9(1), 1-7.
- World Health Organization (WHO) “Tuberculosis and Herbal Medicine: A Review of Current Evidence” World Health Organization (WHO) report.
- Alvarez, A., & Gomez, J. (2014). “A Review on the Role of Herbal Medicines as Adjunctive Treatment in Tuberculosis” Phytotherapy Research, 28(4), 490-503.
- World Health Organization (WHO) “Tuberculosis” World Health Organization (WHO) website
- Centers for Disease Control and Prevention (CDC) “Tuberculosis (TB)” Centers for Disease Control and Prevention (CDC) website
- Pai, M., et al. (2016). “Tuberculosis Diagnosis in the Era of Molecular Technologies” Lancet Infectious Diseases, 16(1), 30-41. DOI: 10.1016/S1473-3099(15)00335-0
- World Health Organization (WHO) Global Tuberculosis Report (2023) “Global Tuberculosis Report 2023” World Health Organization (WHO)
- Raviglione, M. C., & Sulis, G. (2016). “Tuberculosis 2015: Burden, Challenges and Strategy for Control and Elimination” The Lancet, 387(10024), 1097-1108. DOI: 10.1016/S0140-6736(15)00151-7
- Zumla, A., et al. (2015). “Tuberculosis” The Lancet, 386(10010), 2043-2055. DOI: 10.1016/S0140-6736(15)00151-3
- Beyer, J., & Jenkins, P. (2018) “Management of Tuberculosis in Adults and Children” BMJ Best Practice.
- Lawn, S. D., & Zumla, A. I. (2011). “Tuberculosis” The Lancet, 378(9785), 57-72. DOI: 10.1016/S0140-6736(11)60335-4


 Sayyad Kaifali Adam*
Sayyad Kaifali Adam*
 Tejaswini Gurud
Tejaswini Gurud






 10.5281/zenodo.14307877
10.5281/zenodo.14307877