Abstract
Due to impingement upon the corticomedullary junction, retro-odontoid pseudotumor typically cause cervical neck pain or myelopathy. These tumours are characterized by soft tissue development surrounding the longitudinal ligament of the axis. As a sign of atlantoaxial instability, retro-odontoid pseudotumor development is caused by aberrant granulation tissue development, usually posterior to the odontoid process. Dorsal decompression, ventral decompression (both transoral and trans nasal), and other surgical procedures are covered. No more decompression was carried out during the posterior C1-2 fixing procedure. During a year of posterior fixation, there were no noticeable signs, and a follow-up MRI revealed that the ROP had completely resolved with C1-2 bone fusion. With only C1-2 fusion and no decompression, the ROP with C1-2 instability may be completely cured. Discuss about the surgical methods used in the past and now to reduce and eventually reverse a retro-odontoid pseudotumor and pannus. A mass lesion located along the dura posterior to the odontoid process is called a retro odontoid pseudo tumour. Cervical retro-odontoid pseudo myelopathy, a neurological disease, was one of the surgical reasons for the high cervical lateral approach. rheumatoid arthritis-unrelated tumour that is severely squeezing the spinal cord. Ligaments play a crucial part in the CCJ's mechanical stability. Particularly important for controlling the CCJ are the longitudinal and alar ligaments, which connect to the posterior odontoid process. Soft tissue proliferation, also known as pseudotumor, in the area of the transverse ligament of the atlantoaxial (AA) junction has been associated with a wide spectrum of congenital and acquired disorders.
Keywords
Retro-odontoid, Pseudotumor, pannus, corticomedullary junction, Myelopathy, Neurological disease
Introduction
This retro-odontoid pseudo tumoral lesion has been described by multiple authors as synovial cysts, deteriorated transverse ligaments, herniated discs, ganglion cysts, and damaged transverse ligaments. tendons or imitation gout (Cai et al.,2001) (Griesdale et al.,2004). The ligaments surrounding the atlantoaxial junction, leading to long-term inflammation and the development of granulation and fibrotic tissue (Robles et al.,2019) (Fiani et al.,2021). There have been about 70 occurrences of synovial lesions or ganglion lesions at the C1–C2 level documented in the past; all of these cases were connected to atlantoaxial dysfunction or trauma. (Theodotou et al.,2016) (Yang et al.,2021). In 1974, Anderson and D'Alonzo created the first three categories for odontoid fractures connected to pannus development. (Sinha et al.,2017). According to a 1991 theory by Crokard et al., injury to the C1–C2 ligamentous structures causes chronic atlanto-axial instability, which can then cause a retro-odontoid pannus to form. Degenerative articular cysts and non-inflammatory retro-odontoid pseudotumor have been reported in very few occurrences in recent times. (Crokard et al.,1991) (Isono et al.,2001) (Joly et al.,2004) (Tanaka et al.,2010) (Cihanek et al.,2007) (Ito et al.,2000). The brainstem may develop syringomyelia as a result of mechanical displacement, such as morphological changes, (Thornburg et al.,1999) (Spetzler et al.,1988).
Pseudotumor formation can be indirectly caused by a multitude of etiologists. The most common causes are congenital abnormalities such neurofibromatosis, Down syndrome, and Marquee syndrome, as well as rheumatoid arthritis (RA) and severe trauma. When RA is present, inflammatory synovial joint infiltrates cause the posterior longitudinal ligament (PLL) to buckle, which results in the formation of pannus. (Goel et al.,2015). While the method described here may not be novel, it can be regarded as a novel approach to treating retro-odontoid pseudotumor, which are increasingly common in senior patients. Its inclusion in the surgical strategy of posterior cervical fusion or decompression alone is still up for debate (Suetsuna et al.,2006) (Takami et al.,2007). Early detection of cervical myelopathy in the context of an odontoid pseudotumor combined with timely surgical assessment can lower morbidity and enhance results related to spinal cord compression. Furthermore, in order to support patients in maintaining their initial functional state, early intervention is essential (Bakhsheshian et al.,2017).
METHOD AND TECHNIQUES
1] Patients:
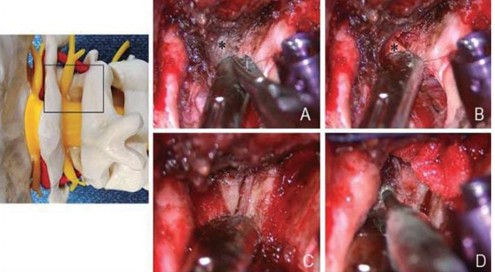
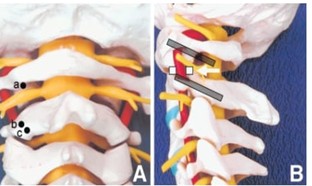
Included were consecutive adult (over 20 years of age) patients who underwent surgery between April 2006 and March 2019 for nonrheumatic pseudotumor. Patients who received treatment for rheumatoid pseudotumor in the same time frame served as the control group. Physicians made the diagnosis of rheumatoid arthritis and gathered data from medical records. Patients who underwent surgery and had a follow-up period shorter than a year were not included. The medical data that was collected included age, sex, previous medical history, cervical pain, neurological signs and symptoms, radiological findings, surgical procedures, difficulties, duration of follow-up, and postoperative symptoms. Neurological signs and symptoms were evaluated using the grip strength test, the grasp-and-release test, the patella tendon reflex, and the modified Rankin Scale (MRS) scores. (Ono et al.,1987). Between 2009 and 2012, five patients who did not have inflammatory illnesses received treatment. All of the patients had irregularities at the cranio-cervical junction and/or lower cervical spondylotic degeneration. There was no proof of atlanto-axial instability. The pre- and post-operative Nurkic scores, pre- and post-operative X-rays, CT scans, and MRIs were all part of the clinical and radiological examination. In one instance, a pannus eggshell calcification was visible on a CT scan. In instances of C0–C1 fusion, all patients had either an occipitocervical fixation (two patients) or a C1–C2 fixation (C1 lateral mass and C2 isthmus-pedicle screws). (Barbagallo et al.,2013). Over the course of three months, a female patient, age 83, developed chronic cervical myelopathy. There was a cystic odontoid mass with a distinct retro-odontoid compressive mass, as shown by computed tomography and magnetic resonance imaging investigations. The transoral extraction was a revolutionary, minimally invasive procedure. Histologic validation of CPPD was acquired. (Klineberg et al.,2014). Three patients (two females and one male) with a cystic retro-odontoid pseudotumor that significantly compressed the spinal cord and was unrelated to rheumatoid arthritis were included in this investigation. 74.7 years old was the mean (range, 73–77 years old). The neurosurgical cervical spine scale (NCSS) was used to evaluate the state of the nervous system.15) At least three months following surgery, a postoperative functional assessment was carried out. (Arima et al.,2019). With the C-2 nerve root sectioned at the C-2 ganglion, the posterior aspect of the C1-2 facet joint was revealed. Anatomical cartilage of the C1-2 facet Bone grafts were placed into the joints after the joint was removed using a high-speed drill. Fig. 1). (Goto et al.,2002).
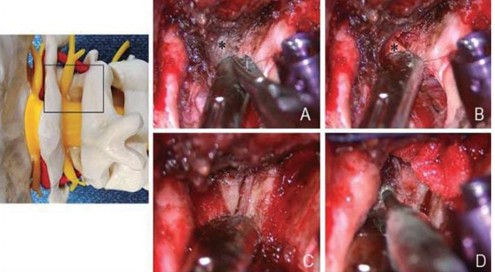
Figure 1: Photos taken during surgery demonstrating the identification and mobilization of the right C-2 nerve root and the placement of a bone graft into the right C1-2 facet joint following the sectioning of the C-2 nerve root.
Surgical Technique:
Cervical retro-odontoid pseudo myelopathy, a neurological disease, was one of the surgical reasons for the high cervical lateral approach. rheumatoid arthritis-unrelated tumour that is severely squeezing the spinal cord. Cases exhibiting clinical symptoms or indicators associated with instability at the C1/2 joints were not considered surgical candidates. In the initial weeks following surgery, a cervical collar was utilized to lessen the patient's suffering. Had slight paralysis of the face and spinal accessory nerves on the side of the surgical approach, which resolved completely approximately a month following the procedure. In every case, the final functional assessment revealed an acceptable or satisfactory level of functional recovery. (Takami et al.,2017). The C-1 lateral mass screw entered the body at the point where the lateral mass and inferior aspect of the C-1 arches met (Fig. 2). The A screw was advanced about 10 degrees medially and superiorly toward the C-1 anterior tubercle while being observed under a fluoroscope. The screws had a diameter of 3.5 mm and a length ranging from 8 to 26 mm (Fig. 3). The C-1 lateral mass screw and the C-2 pars/pedicle screw (SYNTHES, West Chester, PA, USA) were firmly fastened using a rod. The patient was immobilized on the first postoperative day and had to spend several weeks wearing a soft collar. (Takami et al.,2017 a)
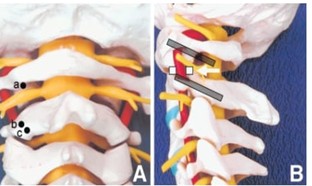
Figure 2A: Photo utilizing a spine model to illustrate the entrance locations for the C-1 lateral mass screw (a), C-2 pedicle screw (b), and C-2 pars interarticularis screw (c). B: A photo displaying the intended sagittal plane screw paths for the C-2 pedicle/pars interarticularis screw and the C-1 lateral mass screw. An arrow points to the bone grafts inserted into the facet joints of the C1-2
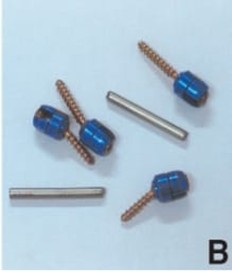
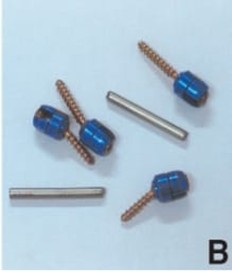
Figure 2B: An image displaying the titanium rods and screws for cancellous bone. The screw has a partially moveable head
Patients were put under general anaesthesia and made to lie horizontal. All patients had posterior fixation, with the exception of those who were severely disabled and at a higher risk of perioperative problems. Altitudinal interval and cervical alignments were taken into consideration during a neurosurgery meeting that determined whether to perform C1-2 fixation or occipitocervical (O-C) fixation on an individual basis. (Niwa et al.,2021). To realign C1 and decompress the spinal cord, the neck was positioned in the neutral position. Patients with AAD who experienced severe spinal cord compression even after being repositioned in the neutral neck position also underwent C1 laminectomy. The iliac crest bone or the C1 lamina were used to create autologous bone transplants (Niwa et al.,2021 a).
Pathophysiology:
Soft tissue proliferation, also known as pseudotumor, in the area of the transverse ligament of the atlantoaxial (AA) junction has been associated with a wide spectrum of congenital and acquired disorders. (Fiani et al.,2021). Three subtypes of RA-associated pannus have been discovered by histopathology; they are known as inflammatory, mixed, and fibrous pannus, respectively. Hyper vascular, hypo vascular, and fibrous pannus are the other names for these subtypes. (Shi et al.,2019). Type II odontoid fractures, which happen where the odontoid base and axis body meet, are the most prevalent kind linked to non-union or malunion. A fibrous mass of soft tissue surrounds the fracture site as a result of malalignment and increased motion at the broken section, which increases the risk of chronic irritation. During 2007. (Anderson and D’ALONZO et al.,1974) (Sinha et al.,2017). Retro-odontoid pseudotumor may occur as a result of inflammatory deposits and amyloid growth. (Wada et al.,2015).
Last but not least, retro-odontoid pseudotumor has been linked to pigmented villonodular synovitis (PVNS) in previous case reports. Up to 36% of cases of PVNS, a proliferative, destructive, non-malignant tumour of synovial membranes, can impact the cervical spine. (Finn et al.,2007) (Roguski et al.,2014). Furthermore, deposition illnesses such gout, amyloid arthropathy, and calcium pyrophosphate dihydrate deposition disease (CPPD) can induce pseudotumor. The underlying disease process of CPPD is called chondrocalcinosis, and it is brought on by calcium pyrophosphate dihydrate crystals that accumulate in the synovium, capsule structures, and tendons (Sekijima et al.,2010).
CLINICAL DISCUSSION
A non-neoplastic lump in the retro-odontoid area that affects seniors is called a pseudotumor. In terms of pseudotumor pathogenesis. (Sze et al.,1986). Eleven of these thirteen instances happened at the craniovertebral junction (CVJ), while two happened at the lower tailbone. This high frequency of dural penetration at the CVJ was not mentioned in any of the previous research. A few earlier investigations have described an unusual dura mater morphology at the CVJ. The two layers that comprise the posterior wall of the thecal sac are the rectus capitis tendon and the outer layer of the cranial dura mater. (Ito et al.,2020). The recommended technique for atlantoaxial fixation has been the C1-2 transarticulaire screw placement; when combined with autologous bone graft and cable, which has a high fusion rate, can completely stop motion at the C1-2 joint. (Magerl et al.,1985) (Dickman and Sonntag et al.,1998) (Haid et al.,2001) (Haid et al.,2001). The AAI's persistent mechanical stress causes transverse ligamentous hypertrophy and recurrent tears, which lead to the development of reactive tissue with fibrous granulation. Most patients have no symptoms at all, though they may report persistent cervical pain. When ROP reaches a serious and mature stage, it may compress the cervical spinal cord and cause neurological problems. Occasionally, a further incident in our case, a ground-level fall can decompensate the clinical state. Pathophysiological, fibrocyte-rich tissue is between the dens and the cross-sectional ligament, or between the odontoid process and the anterior arch of the C1 (Goel et al.,2004) (Yamaguchi et al.,2006). Because the pathology was obvious, total excision of the mass was formerly thought to be the best course of action for treating pseudotumor. Total excision has been achieved using the transoral method, as said by Crokard (Sinha et al.,2017a). The transoral method was thought to be the best course of action for removing the retro-odontoid mass and decompressing the neural structures in individuals with symptomatic spinal cord compression. (Crokard et al.,1986) (Moskovich and Crockard et al.,1990). There isn't a single recommended treatment plan for retro-odontoid pseudotumor. (Sinha et al.,2017b). Took a transoral technique and directly excised the pseudotumor. Previous research has described retro-odontoid pseudotumor as a reactive mass caused by mechanical stress resulting from atlantoaxial instability or ankylosis in the mid and lower cervical spine. For this reason, posterior fusion, such as O-C2 fusion or O-C4 fusion, has been considered the best course of action for halting the pathology's development. Furthermore, the retro-odontoid pseudotumor regressed and the neurological impairments improved following posterior fusion. (Yoshida et al.,1999) (Chikuda et al.,2009). Ligaments play a crucial part in the CCJ's mechanical stability. Particularly important for controlling the CCJ are the longitudinal and alar ligaments, which connect to the posterior odontoid process. (Werne et al.,2019). Though it is still debatable whether the procedure should be included in the surgical approach of posterior cervical fusion or relaxation alone, it can be thought of as an innovative solution for retro-odontoid pseudotumor, which is growing more common in senior patients (Suetsuna et al.,2006a) (Takami et al.,2007a).
Operative Technique:
1] Ventral Decompression:
Many different disorders can cause compression of the front upper cervical spinal cord. The most frequent consequence of compression of the ventral chord that necessitates surgical intervention is the development of an inflammatory pseudotumor. (Joaquim et al.,2019) (Landi et al.,2013) (Oseni et al.,2016). The anterior region of the upper cervical spinal cord can become compressed due to a number of different diseases. Growth of an inflammatory pseudotumor is the most common complication requiring an operation for compression of the ventral cord (Abdelgawaad et al.,2018).
It was demonstrated that the shift in degrees of rotation at C1/C2 caused odontoidectomies to create a redistribution of the axes along which rotation took place. After odontoidectomies, rotation at C1/C2 was reorganized throughout C2's body, resulting in a significant disruption of the body's inherent biomechanics. Although it is much less common, Fig. 3 presents an exemplary case of partial resection of the odontoid and C1. (Fiani et al.,2021a).

Figure 3: An example of a patient with a history of rheumatoid arthritis who presents with bilateral hand paralysis and severe posterior neck pain. (A) Retro-odontoid pannus and compressive upper cervical spinal cord stenosis are seen on preoperative midsagittal T2-weighted magnetic resonance imaging (MRI), in addition to sub axial cervical stenosis. Postoperative trans nasal excision of pannus is shown on (B) postoperative midsagittal T2-weighted MRI. Sub-axial cervical stenosis necessitated additional C1-6 decompressive laminectomy, occipital-T2 instrumentation, and fusion.
There are substantial differences between the access ranges offered by TO and EE techniques. For EE operations, the inferior border is the nasopalatine line (NPL). Even while each patient's NPL may differ depending on their spinal level, the TO technique offers more caudal access than EE surgery. When compared to EEA, the superior border of the TO method is limited. However, this limit can be increased by dividing the hard and soft palates. Conversely, this could lead to velopharyngeal insufficiency (VPI). (Fujii et al.,2015) (Perrini et al.,2014) (Komotar et al.,2012). Rates of VPI in both operations may be underreported since the pathophysiology involves iatrogenic fibrosis of the palate's soft tissue and pharyngeal wall, which may not appear medically for three to six months after surgery. This study showed that underlying illnesses other than rheumatoid pannus could also require surgical treatment. (Shriver et al.,2016)
2. Dorsal Decompression:
Retro-odontoid pseudotumor with symptoms can arise from a variety of aetiologies that do not include intrinsic instability of the cervical or CVJ. In these cases, the posterior treatment alternatives include immediate lesion excision or decrease of the lesion by posterior decompression without fixation. The former has been proven using laminectomy or C1 laminoplasty without the need for any fusion or instrumentation. (Suetsuna et al.,2006b).
Detailed three instances where this method was used to effectively resect nonrheumatic retro-odontoid pannus. Within a minimum of three months and a maximum of two years following surgery, all three patients showed improvement in their symptoms and no recurrence. This approach has several limitations: it cannot achieve complete resection when necessary; it is advised to limit caudal extension to the C3 level; it has a deep and narrow field of view; it poses a risk to the vertebral artery, facial and accessory nerves, and their associated branches; and it becomes necessary to respect the C2 nerve root when it crosses the operative field. But the posterolateral method can still be a good choice for lesions big enough to provide a noticeable mass impact and need direct excision for decompression. (Oohori et al.,2004)
As far back as 1910, a posterior transmural technique for the excision of a lesion situated ventrally was documented in the literature. (Zileli et al.,2020). For a unilateral hemilaminectomy to remove an intradural lesion. Since then, a posterior trans dural technique has been used to treat various extradural ventral lesions such as cysts, retro-odontoid pseudotumor, and herniated discs. (Schomacher et al.,2020)
POSTERIOR INSTRUMENTATION FOR TREATMENT OF PSEUDOTUMOR FORMATION
1] Occipital-Cervical Fusion:
More regression as compared to both anterior and circumferential techniques, as well as similar therapeutic gains in Nurkic score, all while reducing time to recovery and surgical problems (Bydon et al.,2015). Due to the previously described subluxation, individuals usually appear with cases of acute neck discomfort and myelopathy, which might progress to untimely death. (Larsson et al.,1989) (Boden et al.,1993). Odontoid process erosion may also be seen on MRI, which would further suggest posterior instrumentation during surgery because of possible C1-2 instability (Larsson et al.,1989a). When doing occipital surgical fusion, the surgeon uses intraoperative monitoring to evaluate tissue damage while gradually decompressing the medulla to prevent additional pseudotumor progression and to improve neurological results (Sekijima et al.,2010a).
2. C1–2 Fusion:
One of the most frequent areas where pseudotumor development occurs is the C1-2 synovial lining surrounding the odontoid. (Sekijima et al.,2010b). The goal of stabilizing the C1-2 level of the spinal axis is to eventually cause the inflammatory granulation tissue to retreat before neurological symptoms get worse or manifest. (Young and Boyko et al.,2002).
Reducing the longitudinal ligament's gradual deterioration, which would cause the atlas to move forward across the axis and ultimately result in irreversible atlantoaxial kyphosis, is another reason for C1-2 fusion. (Kandziora et al.,1999). The primary advantage of C1-2 fusion is that, compared to transoral/trans pharyngeal resections, it takes a less aggressive strategy and may result in an adequate degree of pseudotumor reabsorption, which could reduce or, in certain cases, completely eliminate neurological signs following surgery as measured by the Nurkic scoring scale. (Bydon et al.,2015a) (Lansen et al.,1990).
CONCLUSION
The pseudotumor was quickly eliminated with occipitocervical fusion, and the clinical symptoms improved favourably. When atlantoaxial causes this illness Joint overload or instability should be treated concurrently with fusion, even if preoperative dynamic imaging shows no signs of instability. Occipital-cervical fusion is the recommended anatomical procedure. There are various justifications for stabilizing C1-2 joints, as well as techniques for doing so, each with a unique set of risks and surgical challenges. Selecting the optimal procedure from the many that have been suggested is challenging because surgeons find it difficult to get enough experience in all of the techniques to make an informed decision. As a result, the theoretical assessment offered here is logical, and the conversation is really beneficial. The pros and cons of placing individual C-1 and C-2 screws versus C1-2 transarticulaire fixation are examined in this patient group afflicted with a retro-odontoid pseudotumor linked to persistent atlantoaxial instability.
REFERENCE
- Cai CY, Palmer CA, Paramore CG. Exuberant transverse ligament degeneration causing high cervical myelopathy. Clinical Spine Surgery. 2001 Feb 1;14(1):84-8. DOI: 10.1097/00002517-200102000-00014
- Griesdale DE Jr, Boyd M, Sahjpaul RL. Pseudogout of the transverse atlantad ligament: an unusual cause of cervical myelopathy. Can J Neural Sci 2004; 31: 273–275. DOI: 10.1017/s0317167100053968
- Robles LA, Mundis GM. Retro-odontoid pseudotumor without radiologic atlantoaxial instability: a systematic review. World Neurosurgery. 2019 Jan 1; 121:100-10. DOI: 10.1016/j.wneu.2018.10.011
- Fiani B, Houston R, Siddiqi I, Arshad M, Reardon T, Gilliland B, Davati C, Kondilis A. Retro-odontoid pseudotumor formation in the context of various acquired and congenital pathologies of the craniovertebral junction and surgical techniques. Neuropile. 2021 Mar;18(1): 67.DOI:10.14245/ns.2040402.201
- Theodotou CB, Urakov TM, Vanni S. Atlantoaxial synovial cyst: case report and literature review. World neurosurgery. 2016 Aug 1; 92:588-e7. Doi: 10.7759/cureus.5377
- Yang MJ, Arkun K, Kryzanski JT: C1-2 cyst presenting with syren globulin: a case report. J Surge Case Rep 2021: rjab097, 2021 Doi: 10.1093/jscr/rjab097
- Sinha P, Lee MT, Panbehchi S, Saxena A, Pal D. Spontaneous regression of retro-odontoid post traumatic cicatrix following occipitocervical fixation. Journal of Craniovertebral Junction and Spine. 2017 Jul 1;8(3):278-82. Doi: 10.14245/ns.2040402.201
- Crokard HA, Sett P, Geddes JF, Stevens JM, Kendall BE, Pringle JA. Damaged ligaments at the craniometrical junction presenting as an extradural tumour: a differential diagnosis in the elderly. Journal of Neurology, Neurosurgery & Psychiatry. 1991 Sep 1;54(9):817-DOI: 10.1136/jnnp.54.9.817
- Isono M, Ishii K, Kamida T, Fujiki M, Goda M, Kobayashi H. Retro-odontoid soft tissue mass associated with atlantoaxial subluxation in an elderly patient: a case report. Surgical neurology. 2001 Apr 1;55(4):223-6. DOI: 10.1016/s0090-3019(01)00345-7
- Joly-Torta M, Martín-Ferrer S, Rimbau-Munoz J, Domínguez C. Reduction of peri odontoid masses following posterior arthrodesis: review of two new cases not linked to rheumatoid arthritis. Neurocrania (Asturias, Spain). 2004 Dec 1;15(6):553-63. DOI: 10.1016/s1130-1473(04)70442-x
- Tanaka S, Nakada M, Hayashi Y, Mohr M, Hayashi Y, Uchiyama N, Hamada JI. Retro-odontoid pseudotumor without atlantoaxial subluxation. Journal of Clinical Neuroscience. 2010 May 1;17(5):649-52. DOI: 10.1016/j.jocn.2009.07.116
- Cihanek M, Fuentès S, Metellus P, Pech-Gourg G, Dufour H, Grisly F. Disparition d’une pseudotumor rétro-odontoïdienne sur instability C1-C2 par osteosyntheses transarticulaire C1-C2. Neurochirurgie. 2008 Feb 1;54(1):32-6. Doi: 10.1016/j.neuchi.2007.12.002.
- Ito T, Hayashi M, Ogino T. Retrolental synovial cyst which disappeared after posterior C1-C2 fusion: a case report. Journal of Orthopaedic Surgery. 2000 Jun;8(1):83-7. DOI: 10.1177/230949900000800115
- Thornburg LE. Ganglions of the hand and wrist. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 1999 Jul 1;7(4):231-8. DOI: 10.5435/00124635-199907000-00003
- Spetzler RF, Hadley MN, Sonntag VK. The transoral approach to the anterior superior cervical spine. A review of 29 cases. InProceedings of the 8 th European Congress of Neurosurgery, Barcelona, September 6–11, 1987: Volume 2 Spinal Cord and Spine Pathologies Basic Research in Neurosurgery 1988 (pp. 69-74). Springer Vienna. DOI: 10.1007/978-3-7091-8978-8_16
- Goel A. Retro-odontoid mass: Evidence of craniovertebral instability. Journal of Craniovertebral Junction and Spine. 2015 Jan 1;6(1):6-7. Doi: 10.4103/0974-8237.151578
- Suetsuna F, Narita H, Ono A, Ohashi H. Regression of retro odontoid pseudotumor following C-1 laminoplasty: report of three cases. Journal of Neurosurgery: Spine. 2006 Nov 1;5(5):455-60. DOI: 10.3171/spi.2006.5.5.455
- Takami T, Goto T, Tugushi N, Nishikawa M, Ohata K. Posterior C1-2 Fixation with Cancellous Screw and Rod System for Retro-odontoid Pseudotumor Associated with Chronic Atlantoaxial Subluxation—Technical Note—. Neurologic medico-chirurgic. 2007;47(4):189-94 DOI: 10.2176/nmc.47.189.
- Bakhsheshian J, Mehta VA, Liu JC. Current diagnosis and management of cervical spondylotic myelopathy. Global spine journal. 2017 Sep;7(6):572-86. DOI: 10.1177/2192568217699208
- Ono K, Ebara S, Fuji TA, Yosenabe KA, Fujiwara KE, Yamashita K. Myelopathy hand. New clinical signs of cervical cord damage. The Journal of Bone & Joint Surgery British Volume. 1987 Mar 1;69(2):215-9. DOI: 10.1302/0301-620X.69B2.3818752
- Barbagallo GM, Certo F, Valsecchi M, Palmucci S, Sciacca G, Albanese V. Disappearance of degenerative, non-inflammatory, retro-odontoid pseudotumor following posterior C1–C2 fixation: case series and review of the literature. European Spine Journal. 2013 Nov; 22:879-88. DOI: 10.1007/s00586-013-3004-1
- Klineberg E, Bui T, Schlenk R, Lieberman I. Retro-odontoid calcium pyrophosphate dehydrate deposition: surgical management and review of the literature. Evidence-based spine-care journal. 2014 Apr;5(01):063-9. DOI: 10.1055/s-0034-1370897
- Arima H, Naito K, Yamagata T, Kawahara S, Ohata K, Takami T. Anterior and posterior segmental decompression and fusion for severely localized ossification of the posterior longitudinal ligament of the cervical spine. Neurologic medico-chirurgic. 2019;59(6):238-45. DOI: 10.2176/nmc.tn.2018-0324
- Goto T, Ohata K, Takami T, Nishikawa M, Tugushi N, Morino M, Matusaka Y, Nishio A, Inoue Y, Hara M. Hydroxyapatite laminar spacers and titanium miniplates in cervical laminoplasty. Journal of Neurosurgery: Spine. 2002 Oct 1;97(3):323-9. DOI: 10.3171/spi.2002.97.3.0323
- Takami T, Naito K, Yamagata T, Kawahara S, Ohata K. Surgical outcomes of posterolateral sulcus approach for spinal intramedullary tumours: tumour resection and functional preservation. World neurosurgery. 2017 Dec 1; 108:15-23. Doi: 10.2176/nmc.tn2012-0419
- Niwa R, Takai K, Taniguchi M. Nonrheumatoid retro-odontoid pseudotumors: characteristics, surgical outcomes, and time-dependent regression after posterior fixation. Neuropile. 2021 Mar;18(1):177. DOI: 10.14245/ns.2040526.263
- Fiani B, Houston R, Siddiqi I, Arshad M, Reardon T, Gilliland B, Davati C, Kondilis A. Retro-odontoid pseudotumor formation in the context of various acquired and congenital pathologies of the craniovertebral junction and surgical techniques. Neuropile. 2021 Mar;18(1):67. Doi: 10.14245/ns.2040402.201
- Shi J, Ermann J, Weissman BN, Smith SE, Mandell JC. Thinking beyond pannus: a review of retro-odontoid pseudotumor due to rheumatoid and non-rheumatoid etiologist. Skeletal Radiology. 2019 Oct 1; 48:1511-23. DOI: 10.1007/s00256-019-03187-z
- Anderson LD, D'ALONZO RT. Fractures of the odontoid process of the axis. JBJS. 1974 Dec 1;56(8):1663-74. PMID: 4434035
- Sinha P, Lee MT, Panbehchi S, Saxena A, Pal D. Spontaneous regression of retro-odontoid post traumatic cicatrix following occipitocervical fixation. Journal of Craniovertebral Junction and Spine. 2017 Jul 1;8(3):278-82. Doi: 10.4103/jcvjs.JCVJS_58_16
- Wada K, Murata Y, Kato Y. Surgical outcome for haemodialysis-related upper cervical lesions. Asian Spine Journal. 2015 Oct;9(5):699. Doi: 10.4184/asj.2015.9.5.699
- Finn MA, McCall TD, Schmidt MH. Pigmented villonodular synovitis associated with pathological fracture of the odontoid and atlantoaxial instability: Case report and review of the literature. Journal of Neurosurgery: Spine. 2007 Aug 1;7(2):248-53. DOI: 10.3171/SPI-07/08/248
- Roguski M, Safin MG, Zerris VA, Kryzanski JT, Thomas CB, Magge SN, Riesenburger RI. Pigmented villonodular synovitis of the thoracic spine. Journal of Clinical Neuroscience. 2014 Oct 1;21(10):1679-85. DOI: 10.1016/j.jocn.2014.03.012
- Sekijima Y, Yoshida T, Ikeda SI. CPPD crystal deposition disease of the cervical spine: a common cause of acute neck pain encountered in the neurology department. Journal of the neurological sciences. 2010 Sep 15;296(1-2):79-82. DOI: 10.1016/j.jns.2010.05.028
- Sze G, Brant-Zawadzki MN, Wilson CR, Norman D, Newton TH. Pseudotumor of the craniovertebral junction associated with chronic subluxation: MR imaging studies. Radiology. 1986 Nov;161(2):391-4. DOI: 10.1148/radiology.161.2.3763907
- Ito K, Yamada M, Horiuchi T, Hongo K. Microanatomy of the dura mater at the craniovertebral junction and spinal region for safe and effective surgical treatment. Journal of Neurosurgery: Spine. 2020 Mar 20;33(2):165-71. DOI: 10.3171/2020.1. SPINE191424DOI: 10.3171/2020.1. SPINE191424 Rogers LC, Payne EE. The dura mater at the cranio-vertebral junction. Journal of Anatomy. 1961 Oct;95(Pt 4):586.
- Magerl FS, Seemann PS. Stable posterior fusion of the atlas and axis by transarticulaire screw fixation. In Cervical spine I: Strasbourg 1985 1987 (pp. 322-327). Vienna: Springer Vienna. DOI:10.1007/978-3-7091-8882-8_59
- Dickman CA, Sonntag VK. Posterior C1-C2 transarticulaire screw fixation for atlantoaxial arthrodesis. Neurosurgery. 1998 Aug 1;43(2):275-80. DOI: 10.1097/00006123-199808000-00056
- Haid Jr RW. C1–C2 transarticulaire screw fixation: technical aspects. Neurosurgery. 2001 Jul 1;49(1):71-4. DOI: 10.1097/00006123-200107000-00011
- Haid Jr RW, Subach BR, McLaughlin MR, Rodts Jr GE, Wahlig Jr JB. C1–C2 transarticulaire screw fixation for atlantoaxial instability: a 6-year experience. Neurosurgery. 2001 Jul 1;49(1):65-70. DOI: 10.1097/00006123-200107000-00010
- Goel A, Phalke U, Cacciola F, Muzumdar D. Atlantoaxial Instability and Retroodontoid Mass—Two Case Reports—. Neuralgia medico-chirurgica. 2004;44(11):603-6. DOI: 10.2176/nmc.44.603
- Yamaguchi I, Shibuya S, Arima N, Oka S, Kanda Y, Yamamoto T. Remarkable reduction or disappearance of retroodontoid pseudotumors after occipitocervical fusion: report of three cases. Journal of Neurosurgery: Spine. 2006 Aug 1;5(2):156-60. DOI: 10.3171/spi.2006.5.2.156
- Crokard HA, Pozo JL, Ransford AO, Stevens JM, Kendall BE, Essigman WK. Transoral decompression and posterior fusion for rheumatoid atlanto-axial subluxation. The Journal of Bone & Joint Surgery British Volume. 1986 May 1;68(3):350-6. DOI: 10.1302/0301-620X.68B3.3733795
- MOSKOVICH R, CROCKARD HA. Posttraumatic atlanto-axial subluxation and myelopathy: Efficacy of anterior decompression. Spine. 1990 Jun 1;15(6):442-7. Doi: 10.1097/00007632-199006000-00002.
- Yoshida K, Hanyu T, Takahashi HE. Progression of rheumatoid arthritis of the cervical spine: radiographic and clinical evaluation. Journal of Orthopaedic Science. 1999 Nov 1;4(6):399-406. Doi: 10.1007/s007760050122.
- Chikuda H, Seichi A, Takeshita K, Shoda N, Ono T, Matsudaira K, Kawaguchi H, Nakamura K. Radiographic analysis of the cervical spine in patients with retro-odontoid pseudotumors. Spine. 2009 Feb 1;34(3): E110-4. doi:10.1097/BRS.0b013e31818acd27
- Werne S. Studies in spontaneous atlas dislocation. Acta Orthopaedical Scandinavica. 1957 Feb 1;28(sup23):3-150.
- Joaquim AF, Osorio JA, Riew KD. Transoral and endoscopic endonasal odontoidectomies–surgical techniques, indications, and complications. Neuropile. 2019 Sep;16(3):462. DOI: 10.14245/ns.1938248.124
- Landi A, Marotta N, Morelli C, Marongiu A, Delfini R. Pannus regression after posterior decompression and occipitocervical fixation in occipital atlanto-axial instability due to rheumatoid arthritis: case report and literature review. Clinical neurology and neurosurgery. 2013 Feb 1;115(2):111-6. DOI: 10.1016/j.clineuro.2012.04.018
- Oseni A, Kakavas G, Scholz M, Petridis A. Case Report: Resolution of a peri odontoid rheumatoid pannus mass in an elderly patient treated with a rigid cervical collar: A case report and literature review. South African Medical Journal. 2016 Jul 19;106(7):687-8. DOI: 10.7196/SAMJ. 2016.v106i7.9861
- Abdelgawaad AS, Kellner G, Elnady B, Ezzati A. Odontoid-sparing trans nasal approach for drainage of craniometrical epidural abscess; a novel technique and review of the literature. The Spine Journal. 2018 Mar 1;18(3):540-6. DOI: 10.1016/j.spinee.2017.12.008
- Fujii T, Platt A, Zada G. Endoscopic endonasal approaches to the craniovertebral junction: a systematic review of the literature. Journal of Neurological Surgery Part B: Skull Base. 2015 Jun 19:480-8. Doi: 10.1055/s-0035-1554904
- Perrini P, Benedetto N, Di Lorenzo N. Transoral approach to extradural non-neoplastic lesions of the craniovertebral junction. Acta Neurochirurgica. 2014 Jun; 156:1231-6. DOI: 10.1007/s00701-014-2057-1
- Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH. Endoscopic skull base surgery: a comprehensive comparison with open transcranial approaches. British journal of neurosurgery. 2012 Oct 1;26(5):637-48. DOI: 10.3109/02688697.2012.654837
- Shriver MF, Kshettry VR, Sindwani R, Woodard T, Benzel EC, Recinos PF. Transoral and trans nasal odontoidectomies complications: a systematic review and meta-analysis. Clinical neurology and neurosurgery. 2016 Sep 1; 148:121-9. DOI: 10.1016/j.clineuro.2016.07.019
- Oohori Y, Seichi A, Kawaguchi H, Tajiri Y, Oda H, Nakamura K. Retroodontoid pseudotumor resected by a high cervical lateral approach in a rheumatoid arthritis patient: a case report. Journal of Orthopaedic Science. 2004 Jan 1;9(1):90-3. DOI: 10.1007/s00776-003-0736-5
- Zileli M, Sharif S, Fornari M, Ramani P, Jian F, Fessler R, Kim SH, Takami T, Shimokawa N, Dechambenoit G, Qureshi M. History of spinal neurosurgery and spine societies. Neuropile. 2020 Dec;17(4):675. Doi: 10.14245/ns.2040622.311
- Schomacher M, Jiang F, Alrjoub M, Witiw CD, Diamandis P, Fehling’s MG. The posterior cervical trans dural approach for retro-odontoid mass pseudotumor resection: report of three cases and discussion of the current literature. European Spine Journal. 2020 Dec; 29:162-70. DOI: 10.1007/s00586-020-06405-8
- Bydon M, Macki M, Qadi M, De la Garza-Ramos R, Kosztowski TA, Sciubba DM, Wolinsky JP, Witham TF, Gokaslan ZL, Bydon A. Regression of an atlantoaxial rheumatoid pannus following posterior instrumented fusion. Clinical Neurology and Neurosurgery. 2015 Oct 1; 137:28-33. DOI: 10.1016/j.clineuro.2015.06.010
- Larsson EM, Holtas S, Zygmunt S. Pre-and postoperative MR imaging of the craniocervical junction in rheumatoid arthritis. American Journal of Roentgenology. 1989 Mar 1;152(3):561-6. DOI: 10.2214/ajr.152.3.561
- Boden SD, Dodge LD, Bohlman HH, Rechtine GR. Rheumatoid arthritis of the cervical spine. A long-term analysis with predictors of paralysis and recovery. JBJS. 1993 Sep 1;75(9):1282-97. DOI: 10.2106/00004623-199309000-00004
- Young WF, Boyko O. Magnetic resonance imaging confirmation of resolution of periodontoid pannus formation following C1/C2 posterior trans articular screw fixation. Journal of clinical neuroscience. 2002 Jul 1;9(4):434-6. DOI: 10.1054/jocn.2002.1092
- Kandziora F, Mittlmeier T, Kerschbaumer F. Stage-related surgery for cervical spine instability in rheumatoid arthritis. European Spine Journal. 1999 Oct; 8:371-81. DOI: 10.1007/s005860050190
- Lansen TA, Kasoff SS, Tenner MS. Occipitocervical fusion for reduction of traumatic periodontoid hypertrophic cicatrix: case report. Journal of neurosurgery. 1990 Sep 1;73(3):466-70. DOI: 10.3171/jns.1990.73.3.0466.


 Mayuri Jagtap*
Mayuri Jagtap*

 10.5281/zenodo.13885121
10.5281/zenodo.13885121